Semi-automated treatment planning for low-dose total body irradiation (TBI)
Ruud van Leeuwen,
The Netherlands
PO-1746
Abstract
Semi-automated treatment planning for low-dose total body irradiation (TBI)
Authors: Ruud van Leeuwen1, Manwel Barsegyan1, Drean Verwegen1, Erik van der Bijl1, René Monshouwer1
1Radboudumc, Radiation Oncology, Nijmegen, The Netherlands
Show Affiliations
Hide Affiliations
Purpose or Objective
Total body irradiation (TBI) is a treatment used in the conditioning of patients prior to hematopoietic stem-cell transplantation. At the department of Radiation Oncology at Radboudumc, an extended source-to-surface distance (350cm), field-in-field technique was developed for TBI. Presently, treatment planning for TBI involves time-consuming forward planning of several multi-leaf collimator (MLC) beams to improve dose homogeneity and decrease dose to organs-at-risk. This research aims to develop and evaluate a computational tool to automatically generate such field-in-field beams for low-dose TBI thereby enabling faster treatment planning.
Material and Methods
Patients were scanned on a CT scanner in supine position, with the knees bent to fit inside the maximum treatment range (160cm). First, the three-dimensional (3D) dose distribution was calculated using the CT scan and the Pinnacle treatment planning system (TPS, Philips, Best, The Netherlands), with two opposing open beams at the treatment distance and gantry and collimator angles. The dose distribution was then exported to our tool, developed in the Python programming language. Using this tool, the 3D dose matrix was projected to the midsagittal plane by calculating the mean along the left-right axis. In the resulting two-dimensional (2D) dose map, four discrete areas (1-4) with similar dose were defined (see Figure 1) using the histogram of the 2D dose map to determine transition dose values. The shapes of these areas were then used to set up four beams including an open beam and three MLC segments to increase the dose in areas 2-4. Monitor units (MUs) for the open beam were calculated aiming to adjust the average dose of area 1 to the prescription dose. For the MLC segments, the aim was to adjust the minimum dose of the corresponding area to the prescription dose. Beams from left and right directions of the patient were mirrored. Beam data were imported in the TPS and the 3D dose was calculated on the CT scan for evaluation. Performance of the software was evaluated quantitatively by analysing dose metrics and adherence to protocol requirements. A qualitative evaluation was carried out in the form of surveys with three experts involved with TBI treatment planning. The survey included a Turing test comparing automated plans and manually created plans, and rating several technical aspects.
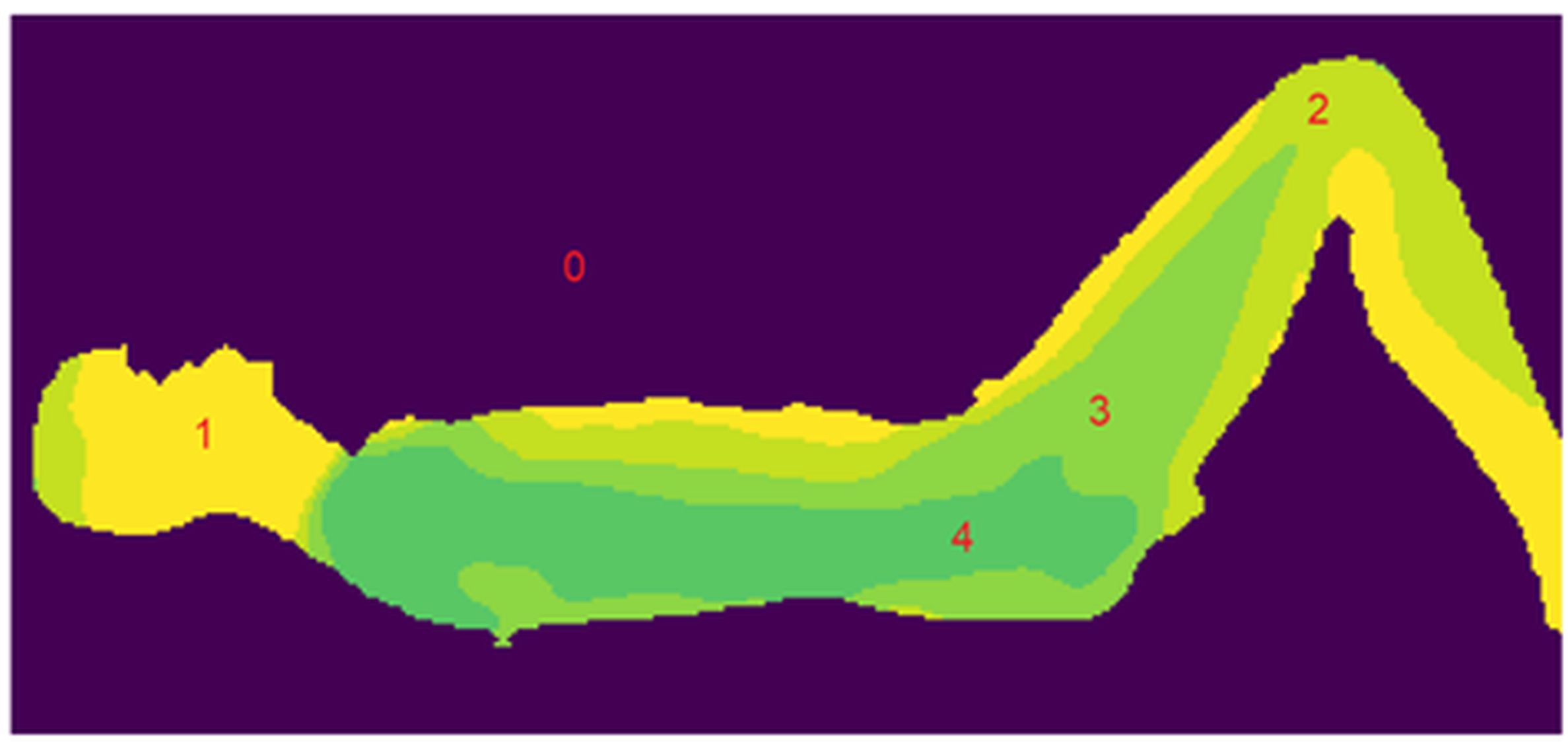
Figure 1. Example of 2D dose map with four dose levels 1-4. A higher level corresponds to a lower dose.
Results
The
quantitative analysis showed that the treatment plans designed by the tool met
protocol requirements. The qualitative surveys showed that the automatically
generated plans are clinically acceptable according to experts. TBI plans could
be produced by the tool within 30 seconds.
Conclusion
We showed that the developed software is successful in creating field-in-field beams for low dose TBI treatment that are acceptable according to protocol requirements and field experts. This method is now part of our standard procedure.