Inter- and intrafraction dose variations in perihilar cholangiocarcinoma SBRT in the STRONG trial
PO-1720
Abstract
Inter- and intrafraction dose variations in perihilar cholangiocarcinoma SBRT in the STRONG trial
Authors: Chiara Paronetto1,2, Wilhelm Den Toom2, Maaike T.W. Milder2, Yvette van Norden2, Rogier Baak2, Ben J.M. Heijmen2, Alejandra Méndez Romero2
1Istituto Oncologico Veneto, Radiotherapy, Padova, Italy; 2Erasmus MC Cancer Institute, Radiotherapy, Rotterdam, The Netherlands
Show Affiliations
Hide Affiliations
Purpose or Objective
Perihilar cholangiocarcinoma patients have mobile tumors that are partly situated outside the liver, with many sensitive organs at risk (OARs) close by. For patients included in the prospective Phase I STRONG trial (NCT03307538), treated with SBRT with respiratory tracking based on fiducials in the liver, we used daily in-room diagnostic repeat CTs (rCT), acquired pre- and post- dose delivery, to analyze inter- and intrafraction dose variations in the target and OARs.
Material and Methods
SBRT was performed with a robotic M6 Cyberknife, connected to an in-room diagnostic CT-scanner on rails using a shared robotic patient couch. Delivered dose was 15x4 Gy at the 80% isodose, planned with a breath-hold exhale planning CT (pCT). For tracking, 2 fiducial markers were implanted in the liver close to the intrahepatic component of the tumor. Five out of 6 analyzed patients had a stent in the central biliary tract (CBT), that was (partly)inside the intra- and extrahepatic target areas. Pre- and post-delivery repeat exhale CTs (rCTs) were acquired in 6/15 fractions. In each of the 72 rCTs, all OARs were re-contoured manually, and the targetwas rigidly copied from the corresponding pCT, using an automated local grey value match with translations and rotations. RCT doses were recalculated for the planned machine settings, using a standalone version of the dose engine in the clinical treatment planning system. To this purpose, rCTswere first matched with their respective pCT using a spine match (translations and rotations), followed by a fiducial match (translations only) to mimick patient setup during treatment.
Results
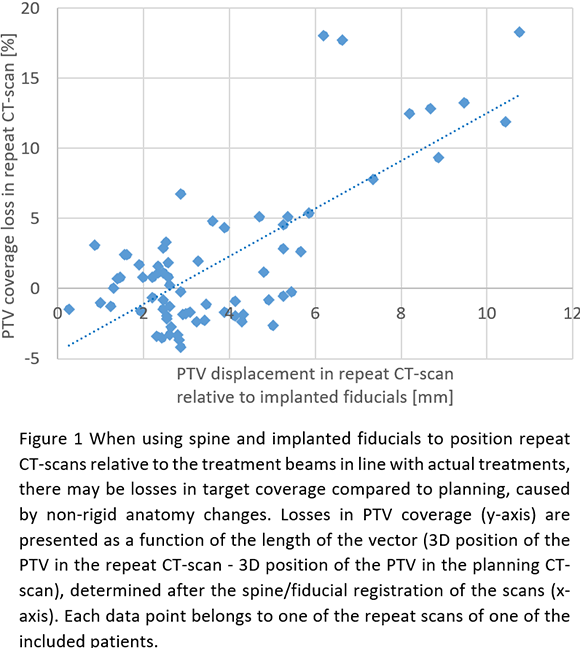
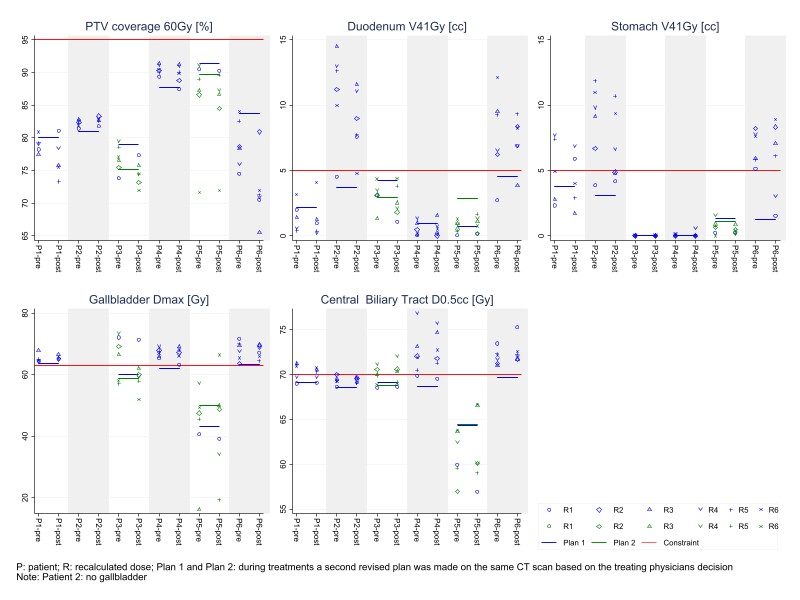
Validity of automatic rigid copying of targets from pCTs to rCTs was confirmed by excellent overlaps between mapped pCT-stents with the corresponding stents in the rCTs. Nonetheless, PTV coverage losses >10% were observed in 2 patients, in 2 and 5 fractions respectively, which were related to displacements of targets in rCTs relative to fiducial center-of-mass (Fig. 1). PTV coverage differences between pre- and post rCTs were on average 2.1% [-3.5,+13]. Large OAR dose increases in rCTs frequently resulted in constraint violations for duodenum, gallbladder, stomach and CBT (Fig. 2), also with occasional ample differences between pre and post rCTs (Fig. 2). Notwithstanding constraint violations observed in the rCTs, we did not register any dose limiting toxicity.
Conclusion
In patients with perihilar cholangiocarcinoma, treated with SBRT using implanted intra-hepatic fiducials for respiratory tracking, we observed large inter- and intrafraction dose deviations in targets and OARs from planning with significant differences among patients. Respiratory motion management based on stents in the central biliary tract, instead of implanted fiducials at a distance in the liver, combined with daily replanning, has promise to enhance treatment accuracy, and is a topic for further research.