Robustness evaluation of surface guided DIBH breast radiotherapy
PO-1710
Abstract
Robustness evaluation of surface guided DIBH breast radiotherapy
Authors: Alessio Gnerucci1, Serenella Russo2, Marco Esposito2, Alessandro Ghirelli2, Silvia Pini2, Lisa Paoletti3, Raffaella Barca3, Simona Fondelli3, Paolo Alpi3, Barbara Grilli3, Francesca Rossi4, Slvia Scoccianti3
1University of Florence, Physics and Astronomy, Florence, Italy; 2Azienda USL Toscana Centro, Medical Physics Unit, Florence, Italy; 3Azienda USL Toscana Centro, Radiotherapy Unit, Florence, Italy; 4Azienda USL Toscana Sud Est, Radiotherapy Unit, Grosseto, Italy
Show Affiliations
Hide Affiliations
Purpose or Objective
Aim of this work was to assess the robustness of a DIBH technique based on optical surface tracking technology for patients undergoing adjuvant RT for left sided breast cancer.
Material and Methods
Ten patients were enrolled in this study. 3D conformal technique for 42,56Gy dose in 16 fractions was adopted. C-RAD Sentinel™ laser scanning system and a Siemens CT scanner were used for the prospective DIBH CT study. Base line and gating window levels (5mm amplitude) were established during CT simulation procedure. Gated treatments delivery was supported by the C-RAD Catalyst™ system connected with an Elekta Synergy. Residual isocenter shifts were tracked in real time by matching the live surface with a daily reference with a threshold for beam triggering set to 5 mm.
The intrafraction motion evaluation was performed by investigating the residual isocenter shifts during beam on time for the lateral, longitudinal and vertical directions for each treatment fraction. Mean and SD of the residual isocenter shifts over all the treatment fractions of each patient were calculated.
Plan robustness was evaluated, for each patient, by calculating the perturbed dose for the single-fraction plan in accordance with the daily residual isocenter shift. Perturbed plans were then accumulated in the overall “shifted” treatment plan. Shifted and original plans were compared in terms of the main DVH goals for target coverage and OARs doses. Statistical significance of dosimetric data was analysed using a Wilcoxon signed-rank test considered significant if p<0.05.
Results
The residual isocenter shifts during beam on time for 160 treatment fractions were calculated. Intra-fraction mean isocenter shifts over all the patients were 0.1±0.7 mm, -0.6±0.9 mm, 0.3±0.2 mm and 2.4±0.5 mm for lateral, longitudinal, vertical, and deviation respectively with a maximum-minimum range of -1.1÷1.3 mm, -2.2÷1.1 mm, -1.3÷0.4 mm and 1.6÷3.3 mm respectively.
In fig. 1 is reported an example of the shifts investigation for a single patient: both the average shift vector for each fraction and the cumulative residual shifts distributions are shown.
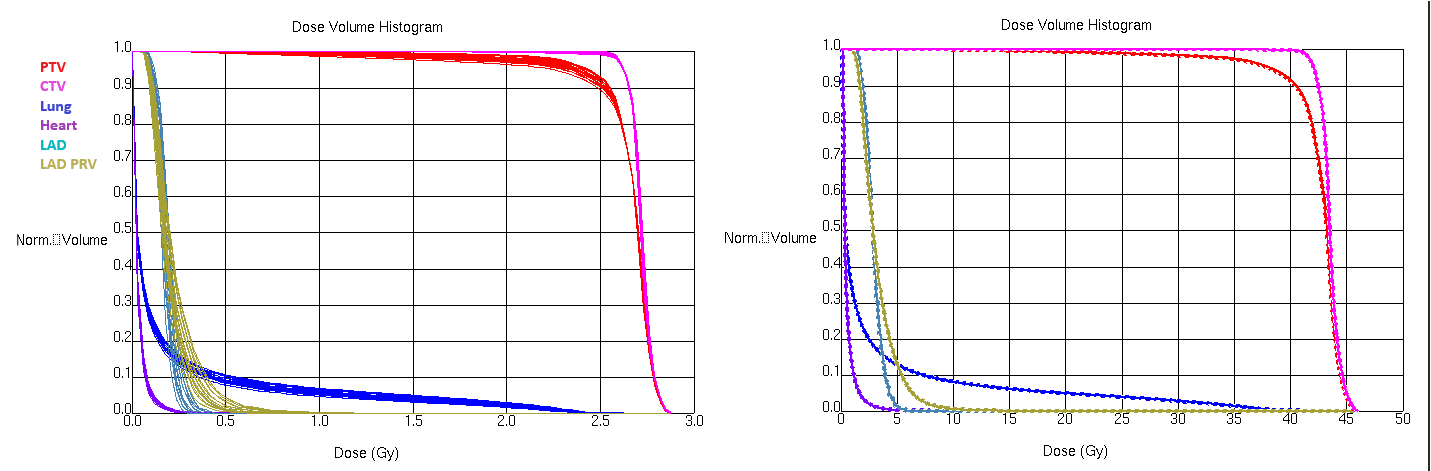
The average DVH variations due to residual isocenter shifts over all the patients were: 0.0±0.4% for PTV 95% coverage; 0.02±0.06Gy and 0.9±1.9Gy for the mean and maximum(1cc) Heart dose respectively; 0.2±0.3Gy and 0.5±0.8Gy for the mean and maximum LAD PRV dose respectively and 0.4±0.5% for Sx Lung 20Gy volume. For each DVH goals any significant dosimetric difference between the shifted and the original plan was found, this indicating that the technique and its planning and margin definition strategy is robust.
An example of the daily and total plan DVH variation for a single patient is reported in fig. 2.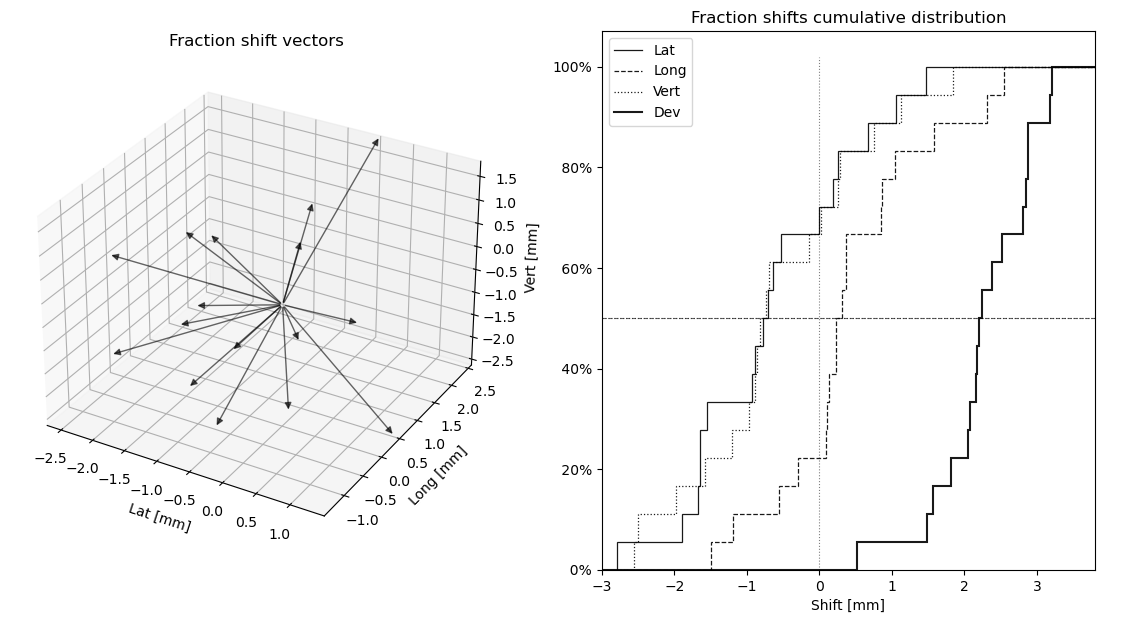
Conclusion
DIBH procedure guided by optical systems for left breast irradiation is a reproducible and stable technique with a limited intra-fraction DIBH variability. Residual isocenter shifts do not produce significant dosimetric variations, assessing the robustness of the treatment strategy.