Visibility, artifacts and dose degradations around gold markers in proton therapy of prostate cancer
Liliana Stolarczyk,
Denmark
PO-1682
Abstract
Visibility, artifacts and dose degradations around gold markers in proton therapy of prostate cancer
Authors: Liliana Stolarczyk1, Jesper Folsted Kallehauge1, Lia Barbosa Valdetaro1, Ludvig P. Muren1, Morten Høyer1, Pia Randers2, Tanja Stagaard Johansen1, Heidi S. Rønde1, Mateusz Sitarz1, Sofie Tilbæk1, Anne Vestergaard3, Lise Bentzenb4, Stine Elleberg Petersena5
1Aarhus University Hospital, Danish Center for Particle Therapy, Aarhus, Denmark; 2Aarhus University Hospital, Danish Center for Particle Therapy, , Aarhus, Denmark; 3Aarhus University Hospital, Aarhus, Danish Center for Particle Therapy, , Aarhus, Denmark; 4Aarhus University Hospital, Department of Oncology,, Aarhus , Denmark; 5Aarhus University Hospital, Aarhus, Denmark, Danish Center for Particle Therapy, Aarhus, Denmark
Show Affiliations
Hide Affiliations
Purpose or Objective
Implantation of fiducial markers may potentially expand image-guidance strategies in proton therapy of prostate cancer. However, markers may cause imaging artefacts, and more importantly degradation of the dose distribution of proton beams passing through a high-density marker. As a part of a national randomised trial (PROstate PROTON trial 1) where proton therapy will be delivered concomitantly to the prostate, seminal vesicles and pelvic lymph nodes, we therefore evaluated different commercially available fiducials with respect to their visibility in selected imaging modalities and dose degradation downstream of the markers.
Material and Methods
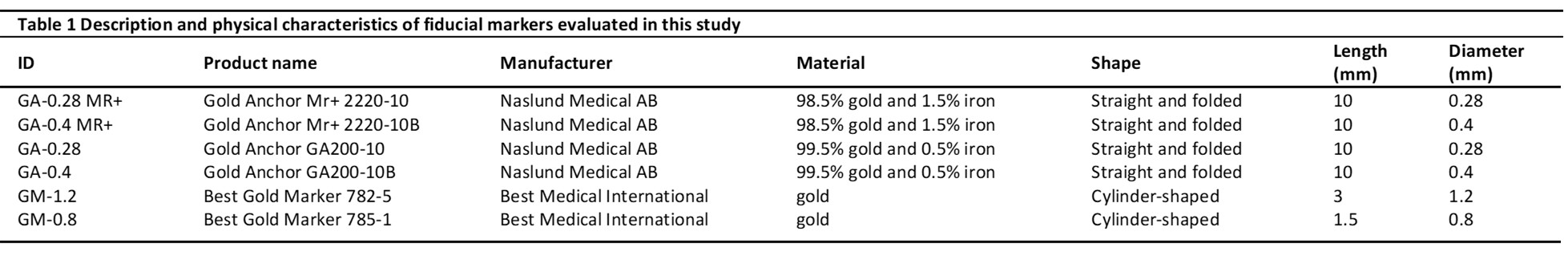
Best Gold Markers (GM) and Gold Anchor (GA) fiducials of different forms and sizes (Table 1) were assessed. Comparison was performed for markers already used in proton RT as well as for a recently developed GA with increased content of iron in the alloy (GA MR+). Markers were implanted in animal tissue positioned inside the Gammex (CIRS) phantom. The phantom underwent CT scanning (Siemens Somatom Definition Edge), magnetic resonance imaging (Philips Ingenia 3T), 2D kV imaging and cone-beam CT scanning (CBCT, ProBeam Varian). Visibility of different markers was assessed qualitatively through visual inspection. The dose distribution downstream of the markers positioned parallel to proton beam was evaluated using EBT3 films (Ashland) in the entrance, in the plateau and at the end of a spread-out Bragg peak (SOBP) with energies ranging from 160 to 190 MeV. Additional dose measurements were obtained with 3D radiochromic dosimeters for the GA-0.4 marker commonly used in proton RT.
Results
The best trade-off between CT image quality, marker visibility and artefacts was obtained for the pelvic protocol (Twin Beam, AuSn 120kV, 2 mm slice thickness, applied iMAR algorithm). The smallest artefacts were observed for GA-0.28, GA-0.28 MR+ and GM-0.8. The content of iron did not influence the quality of CT images. All markers, except for GM-0.8 mm, were visible on 3D T2w-MRI scans performed with the clinical pelvic protocol. GA-0.28 MR+ had a better image-contrast in comparison to GA-0.28 (Figure 1). All markers were clearly visible on CBCT and orthogonal kV images. With respect to dose degradations, the largest underdosage was measured at the end of the SOBP and was at the level of 30%, 10% and 5% for GM-1.2, folded GA-0.4 and folded GA-0.28, respectively. The dose degradations were equivalent between markers with different iron content. The shadowing effect was substantial more than 10 mm downstream of markers.
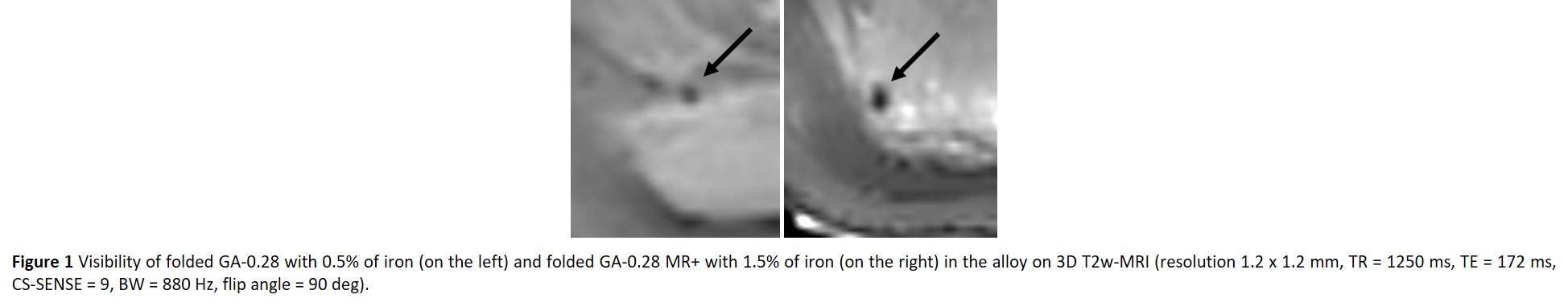
Conclusion
All tested markers gave clear signal on CT and CBCT scans. GM-1.2 caused intolerably high dose degradation and therefore was excluded from the usage in the proton part of our trial. The smallest shadowing effect was measured for GM-0.8 and GA-0.28. In connection with the improved visibility on MR scans GA-0.28 MR+ gives promising results for future clinical use in proton RT.