Catching errors by synthetic CT in the clinical workflow of an MR-Linac
PO-1554
Abstract
Catching errors by synthetic CT in the clinical workflow of an MR-Linac
Authors: Jie Li1, Bin Tang1, Min Liu1, Sichuan Guo2, Xinghong Yao1, Xiongfei Liao1, Xi Feng1, Lucia Clara Orlandini1
1Sichuan Cancer Hospital & Institute, Radiotherapy Department, Chengdu, China; 2Elekta Instrument (Shanghai) LTD, MR-Linac Clinical Operation, Shanghai, China
Show Affiliations
Hide Affiliations
Purpose or Objective
In the clinical workflow of a 1.5 MR-linac, it is possible to adapt to shape (ATS) the contours and reoptimize the plan by using the synthetic computed tomography (syCT) of the daily magnetic resonance imaging (MRI). This study aims to evaluate the minimum dosimetric errors expected in the ATS workflow while recalculating a plan on a syCT.
Material and Methods
Twenty patients treated at 1.5T MR-Linac in different tumor sites i.e., prostate (1), pancreas (1), rectum (3), cervix (4), liver (5), vertebra (1), brain (1), pelvis (1), kidneys (2), lung (1), were consecutively included in this retrospective study. Each patient underwent a CT simulation scan with arms above head using indexed patient positioning aids. The patient’s target and OARs were contoured in Monaco V5.4, and a reference plan was generated using ten to twelve individual beam angles. The reference plan ready-to-use in the ATS workflow contains all the density bulk assignment information i.e., the contours to use and their corresponding average electronic density (ED), the priority of each contour respect to density assignment in case of contour overlaps. To assess the dosimetric error made by using ATS procedure, the plan is recalculated on ideal syCT imaging obtained from the reference CT by forcing the drawn contours to the average ED as defined on reference plan. Targets and organs at risk (OAR) dose-volume histogram (DVH) of the CT and syCT plans as well as the dose distributions using gamma analysis 3%-3mm and 2%2mm criteria, were compared.
Results
For the dose distribution on syCT and CT, the average pass rate of gamma analysis using the 3%/3 mm and 2%/2 mm criteria were higher than 99% and 98%, respectively for 16 patients out of 20; similarly targets and OARs DVH dose differences remained below 1%. A representative patient CT and syCT and corresponding DVHs in good agreement are displayed in Figure 1. For the remaining 4 patients, the source of discrepancy was investigated, and the CT reference plan was reworked to decrease the dosimetric differences on the syCT plan; the results achieved are shown in Table 1. For the lung case, the dosimetric difference remained high and the patient was treated in adapt to position instead of ATS.
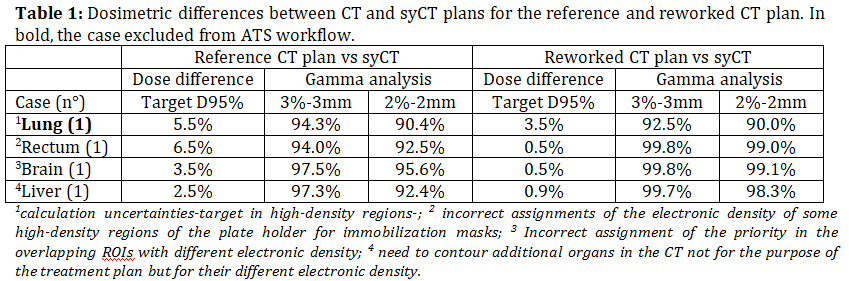
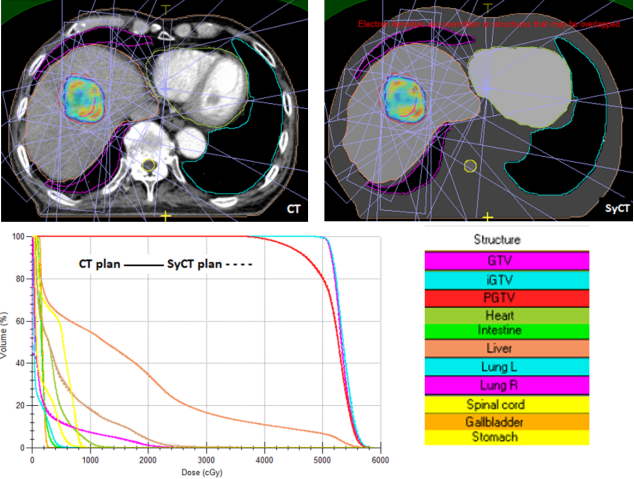
Figure 1. A representative patient CT and SyCT and corresponding dose volume histograms.
Conclusion
The syCT should be investigated before its use for each new treatment planning, as factors including involuntary errors in the optimization procedures, high gradients in the treatment fields, and the need to increase the contours used in the force ED process, can affect the accuracy of the plan dosimetry.