Adjuvant radiotherapy after salvage surgery for recurrent nodal melanoma
Lodewijka HJ Holtkamp,
The Netherlands
PO-1438
Abstract
Adjuvant radiotherapy after salvage surgery for recurrent nodal melanoma
Authors: Lodewijka HJ Holtkamp1,2, Serigne N Lo1,3, John F Thompson1,3,4, Omgo E Nieweg1,3,4, Angela M Hong1,3
1The University of Sydney, Melanoma Institute Australia, Sydney, Australia; 2University Medical Center Groningen, Department of Surgical Oncology, Groningen, The Netherlands; 3The University of Sydney, Faculty of Medicine and Health, Sydney, Australia; 4Royal Prince Alfred Hospital, Department of Melanoma and Surgical Oncology, Sydney, Australia
Show Affiliations
Hide Affiliations
Purpose or Objective
Adjuvant radiotherapy (RT) to a regional lymph node field has a potential role following an initial elective lymph node dissection in high-risk stage III melanoma patients, but is also used after resection of a node field recurrence following a prior node dissection. The efficacy of RT in these two clinical scenarios may differ. In the second scenario, where the tumour biology may have become more aggressive, the value of adjuvant RT is less evident. The purposes of this study were to determine node field control and recurrence-free (RFS), melanoma-specific (MSS) and overall survival (OS) rates after adjuvant RT in a cohort of these latter patients in an era before effective systemic immunotherapy became available.
Material and Methods
Seventy-six patients who received adjuvant nodal RT after excision of node field recurrence following a previous node dissection between 1990 and 2011 were identified from the Melanoma Institute Australia database. The RT fractionation schedule (conventional fractionation or hypofractionation) was at the discretion of the treating radiation oncologist.
Results
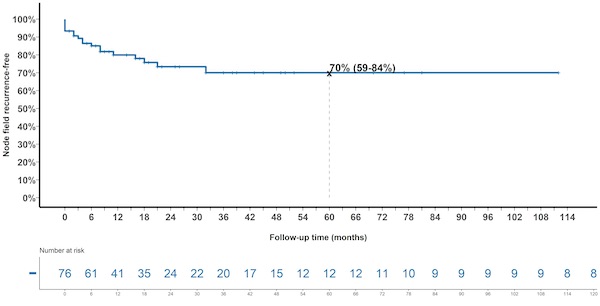
Dissected lymph node fields were axilla (49%), groin (26%) and neck (25%). The median time to diagnosis of node field recurrence after initial nodal dissection was eight months (range 23 days-17 years). Salvage surgery varied from local excision of the recurrence to a “re-do” lymph node dissection, as considered appropriate for the individual patient. Involved surgical margins were reported in 19 patients (25%), and lymph nodes with extra-nodal spread in 18 (24%). Adjuvant RT with conventional fractionation (median dose 48 Gy in 20 fractions) was given to 43 patients (57%) and hypofractionated RT (median dose 33 Gy in 6 fractions) to 33 patients (43%). The median follow-up duration was 19 months (range 1-246 months). The five-year node field control rate was 70% (95% CI 59-84%) (figure), five-year RFS 17% (95% CI 10-29%), five-year MSS 26% (95% CI 18-39%) and five-year OS 25% (95% CI 17-38%).
Conclusion
Despite the recurrence and the presence of high-risk features such as a positive margin in 25% of patients and extranodal spread in 24% of patients, node field control was achieved in 70% of patients. Therefore melanoma patients with resected isolated melanoma node field recurrence after a previous dissection may benefit from adjuvant RT. However, disease progression at distant sites was common and survival outcomes were poor. Unfortunately, comparing our node field control rate after salvage surgery and adjuvant RT with a cohort treated with salvage surgery without RT was not feasible due to very low number of patients. Prospective data to assess the role of adjuvant RT in the setting of systemic therapy with checkpoint inhibitors or targeted therapy is required to guide treatment decisions in this subgroup of patients at high risk of nodal as well as distant recurrence.