Is it possible to deliver on-line MR-guided RT for prostate cancer within a feasible time frame?
PO-1421
Abstract
Is it possible to deliver on-line MR-guided RT for prostate cancer within a feasible time frame?
Authors: Tine Schytte1, Pia Krause Møller1, Uffe Bernchou2, Karina L Gottlieb3, Ebbe Laugaard Lorenzen4, Soren Agergaard2, Henrik R Jensen3, Christina Junker Nyborg1, Lars Dysager1, Olfred Hansen5, Faisal Mahmood2, Rana Bahij5, Carsten Brink2, Anders Smedegaard Bertelsen3
1Odense University Hospital, Oncology, Odense , Denmark; 2Odense University Hospital, Laboratory of Radiation Physics, Odense, Denmark; 3Odense University Hospital, Laboratory of Radiation Physics, Odense , Denmark; 4Odense University Hospital, Laboratory of Radiation Physics, Odense University Hospital, Denmark; 5Odense University Hospital, Oncology, Odense, Denmark
Show Affiliations
Hide Affiliations
Purpose or Objective
The PRISM-OUH protocol (Prostate
Radiotherapy Integrated with Simultaneous MRI) has included patients with
localized prostate cancer treated on the 1.5 T MR-linac (Unity, Elekta AB,
Stockholm, Sweden). The protocol aimed to assess the feasibility, safety, and
tolerability of the adaptive treatments. The primary endpoint was to evaluate
whether on-line MR-guided radiotherapy (oMRgRT) could be delivered within a clinically
feasible time-period (more than 90% of the fractions (F) delivered within 60minutes).
This study reports the treatment times from PRISM as well as time
evolution of the manuel tasks during the study.
Material and Methods
Localized prostate
cancer patients were included from December 2018-to April 2020. Radiotherapy
(RT) was planned to a total dose of 60 Gy in 20 F to the prostate and proximal
1cm of the seminal vesicles (SV), 48 Gy was given to an additional 1cm of the
SV. The PTV margins were 5mm isotropic, except for 3mm posteriorly PTV 60 Gy. Organs
at risk (OAR) were bladder, rectum, and bowel. Prostate, SV, and OAR were
registered from the reference plan to the daily MR scan and manually adjusted
if needed.
At each fraction, the total
session time (in-room time) was registered together with time used for image
fusion and conturing.
Two different types of workflow were used: Adapt-to-position (ATP) that
used rigid contur propagation registration and translation of treatment fields,
and adapt-to-shape (ATS) that uses deformable propagation of conturs, contur
correction and a full treatment re-planning.
Results
The trial included 31
patients with a median age of 69 years (46-76), Gleason scores 6-7, and 78% had
performance status 0. Of the planned 620 F, 26 F were delivered on standard
linac (15: one patient had claustrophobia, 11: technical problems). The median in-room time and range were 25 (18–62)min for ATP, and 35 (21–69)min for ATS (fig 1a). The majority of the fractions (590/594) were delivered within 60 min. Treatment interruption with the need to have the patient off the couch occurred at 25 fractions (8: technical issue, 17: large filling of the rectum). In all cases, these treatments were delivered later during the same day.
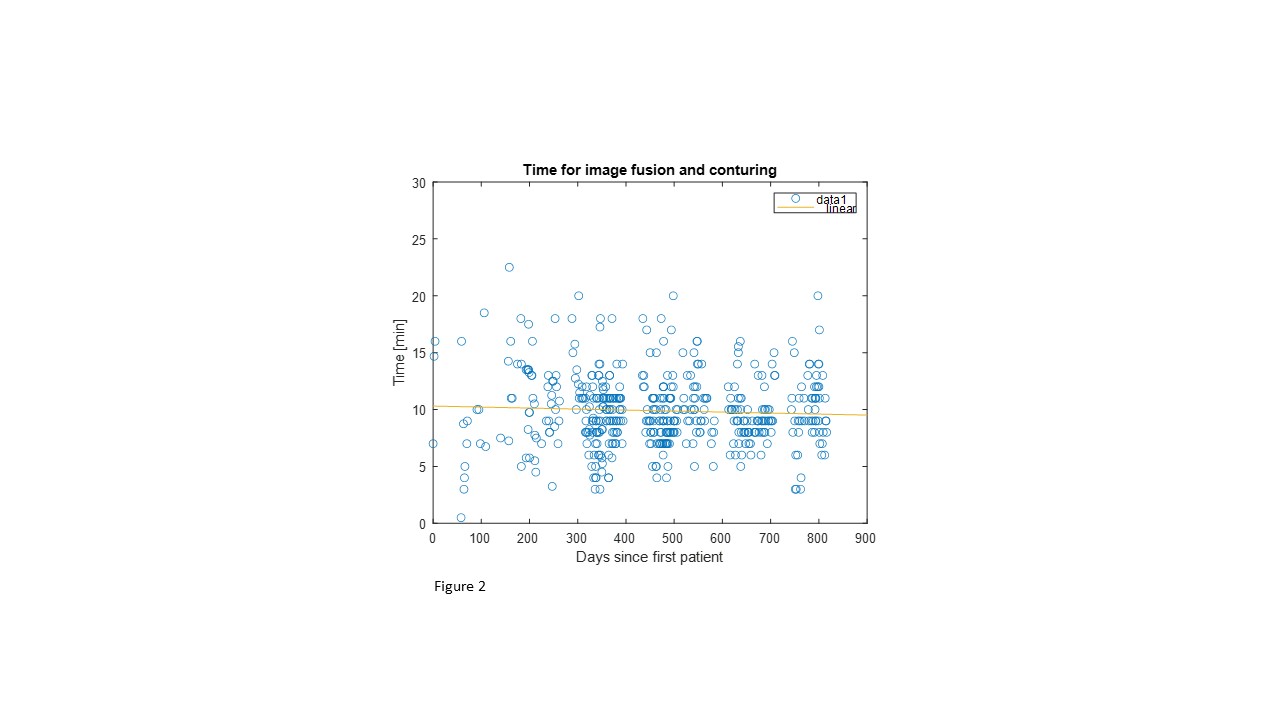
The median time for manual image registration and contouring was 2 min, range (1–11)min for ATP, and 9 min, range (1–35)min for ATS (fig 1b). There was no indication of decreased delineation time over the study period (fig 2).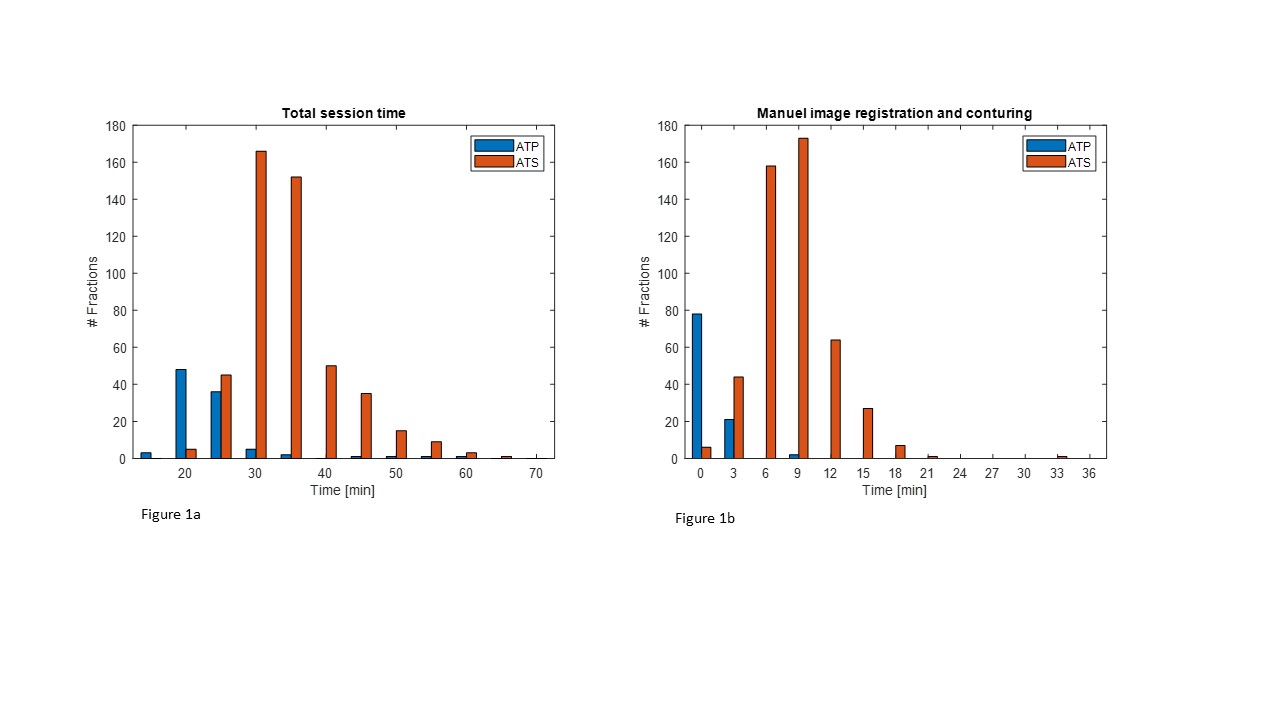
Conclusion
From this study, we conclude that it is feasible to deliver daily oMRgRT
for patients with prostate cancer since 99.3% of the fractions were delivered
within 60min. The simpler ATP workflow is significantly faster to deliver than
ATS that utilizes all the adaptive planning advantages. Surprisingly, the time needed for the
time-cosuming manual image registration and contouring has not declined over
time; this might partly be due to the training of new staff during the study
period. Improved deformable image registration algorithms are needed to reduce
the treatment time significantly.