Number of PSMA-PET positive lymph nodes affects outcome in node positive prostate cancer patients
PO-1411
Abstract
Number of PSMA-PET positive lymph nodes affects outcome in node positive prostate cancer patients
Authors: Simon Spohn1,2,3, Viktoria Birkenmaier1, Juri Ruf4, Tanja Sprave1,2, Anca Grosu1,2, Constantinos Zamboglou1,2,3,5
1University Medical Center Freiburg, Department of Radiation Oncology, Freiburg, Germany; 2German Cancer Consortium (DKTK), Partner Site Freiburg, Freiburg, Germany; 3Faculty of Medicine - University of Freiburg, Berta-Ottenstein-Programme, Freiburg, Germany; 4University Medical Center Freiburg, Department of Nuclear Medicine, Freiburg, Germany; 5European University of Cyprus, German Oncology Center, Limassol, Cyprus
Show Affiliations
Hide Affiliations
Purpose or Objective
National comprehensive cancer network recommends external beam radiotherapy (EBRT) combined with androgen deprivation therapy (ADT) for newly diagnosed node positive (cN1) prostate cancer (PCa) patents as the preferred treatment option. Despite heterogeneous outcomes, risk stratification does not incorporate further differentiation such as number of positive nodes. Furthermore, implementation of positron emission tomography targeting prostate specific membrane antigen (PSMA-PET) in staging of primary PCa patients, challenges former retrospective analyses and TNM stage differentiation between cN1 and cM1a. This study aims to evaluate outcomes of PSMA-PET node positive (cN1 and cM1a) PCa patients after EBRT.
Material and Methods
Data of fifty patients with cN0 and/or cM1a PCa staged by PSMA-PET were retrospectively analyzed. All patients had received EBRT to the pelvis ± boost to positive nodes, followed by boost to the prostate. Predictive factors for biochemical recurrence-free survival (bRFS) (Phoenix-criteria) and metastases-free survival (MFS) were analyzed by univariate- and multivariate Cox regression and Kaplan-Meier plots. Doses delivered to the prostate, elective lymph nodes and PSMA-positive nodes, as well as genitourinary (GU) and gastrointestinal (GI) toxicities were assessed.
Results
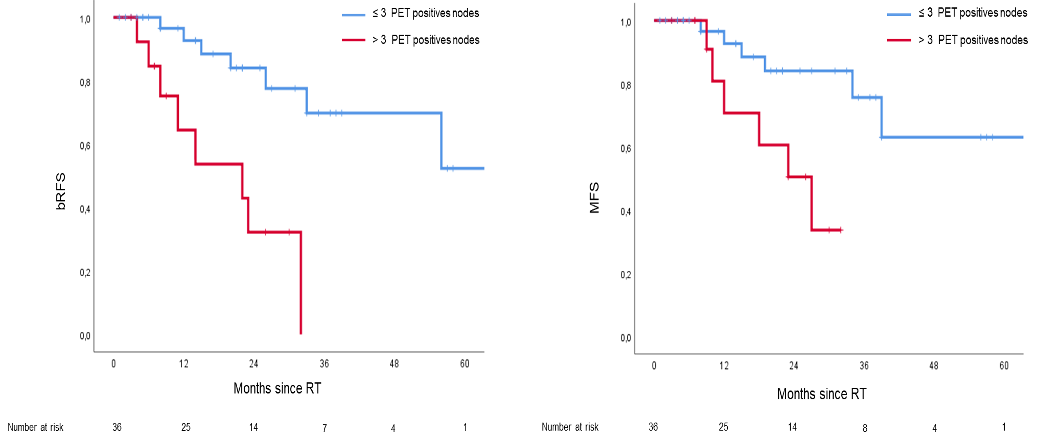
Median follow up was 24 months (IQR 8-38). Median age was 75 years and initial PSA was 19.5 ng/ml. Most patients (90%) had cT stage ≥ 2c and ISUP grade ≥ 3 (86%). Median dose to the prostate, elective nodes and PET-positive nodes were 75Gy (IQR 74-76), 45 Gy and 55 Gy, respectively. 90% of patients received ADT with a median duration of 8.5 months (IQR 6-18). Chronic ≥ grade 2 GU and GI toxicities were 6% and 4%. In contrast to clinicopathological features, cM1a stage and number of positive pelvic nodes in PET (n=0-3 vs n>3) were significantly associated with bRFS in univariate analysis and number of positive lymph nodes remained significant in multivariate analysis. (p=0.01). Number of pelvic positive nodes was also significantly associated with MFS (p=0.02).
Figure 1: Biochemical recurrence free survival and metastases free survival according to > 3 PET-positive lymph nodes
Conclusion
Our results support the need for stratification of PSMA-PET node positive patients. Tumor burden in terms of number of positives nodes might be a relevant prognosticator for bRFS and MFS and guide treatment de- and escalation. This hypothesis should be evaluated in larger cohorts.