85 patients with BCR following RP (pN0-pNx) plus
PB-RT and staged with PSMA-PET between June 2016 and October 2020 were included
in the present analysis. PB-RT was performed as adjuvant RT (ART) in 27 pts: 26
(96,3%) had a p-staging ³ pT3 (15 pT3a, 11 pT3b) and 24 (88,8%) had R+. The
remaining 58 pts had received salvage RT (SRT), with a median pre-treatment PSA
of 0,47 ng/ml (range 0,10 – 3,3). Overall, 14 pts had received ADT along with
PB-RT. The median interval from the end of PB-RT to subsequent BCR was 35,1
months (range 1 – 153).
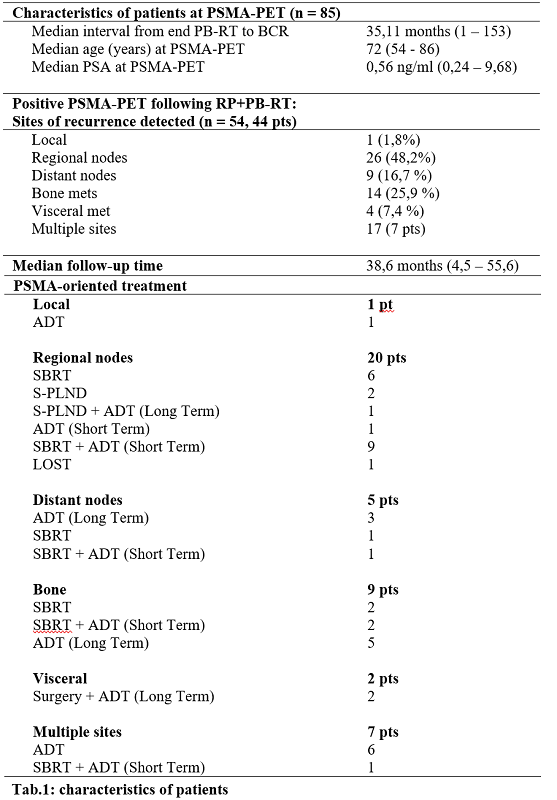
The median PSA at PSMA-PET was 0,56 ng/ml (range 0,24 – 9,68). PSMA-PET was
positive in 44 patients (75,86%): 27/58 SRT (46,5%) and 17/27 ART
(62,9%). Fifty-four lesions were detected. The most common site (48,2%) was regional nodal: 26
lesions in 20 pts [Tab.1]. Positive PSMA-PET oriented treatment was: ADT (Arm-1)
for 15 pts (34%), SBRT/Salvage-Pelvic Lymph Node Dissection (S-PLND) (Arm-2)
for 11 pts (25%), and SBRT/S-PLND + ADT (Arm-3) for 16 pts (36,4%) [Tab.1].
Details about treatment per failure-site are reported
in Tab.1.
No treatment data
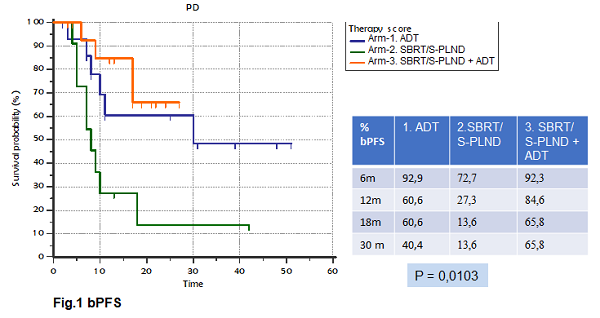
were available for 2 pts after positive PSMA-PET. The median bPFS following any
treatment guided by positive PSMA-PET was 10,9 months (range 2 – 50,8) [Fig.1].
Overall, 32 pts (72,7%) received ADT: 13 short term (40,6%); and 17 (53,1%) long
term, of whom 15 still undergoing ADT. Among those treated exclusively with
SBRT (9/44, 20,5%), 7 recurred (77,8%) with a median bPFS of 7,8 months (range
4,4 – 18,12). For the 2 pts not relapsed after exclusive SBRT, the median ADT-free
survival was 27,3 months (12,6 – 42). Overall, just 1 death was recorded (other
cause). The median observation time from PSMA-PET to the last follow-up
following PSMA-oriented treatment was 38,6 months (range 4,5 – 55,6).
A statistically significant difference (p = 0.01) in terms of bPFS was recorded
between Arm-1, Arm-2 and Arm-3: at 30 months bPFS was 40,4% for Arm-1, 13,6%
for Arm-2 and 65,8% for Arm-3 [Fig.1]