Impact of Statin Use on Biochemical Failure following Radical Prostatectomy or Radiation Therapy
PO-1395
Abstract
Impact of Statin Use on Biochemical Failure following Radical Prostatectomy or Radiation Therapy
Authors: Linda Huynh1, Emily Keit1, Raymond Carrillo2, Erica Huang2, Thomas Ahlering2, Shawna Boyle3,3, Charles Enke1, Michael Baine4
1University of Nebraska Medical Center, Radiation Oncology, Omaha, USA; 2University of California Irvine, Urology, Orange, USA; 3University of Nebraska Medical Center, Urology, Omaha, USA; 4University of Nebraska Medical Center, Radiation oncology, Omaha, USA
Show Affiliations
Hide Affiliations
Purpose or Objective
To assess the impact of statin use on overall and time to biochemical failure following primary treatment of localized prostate cancer (PC)
Material and Methods
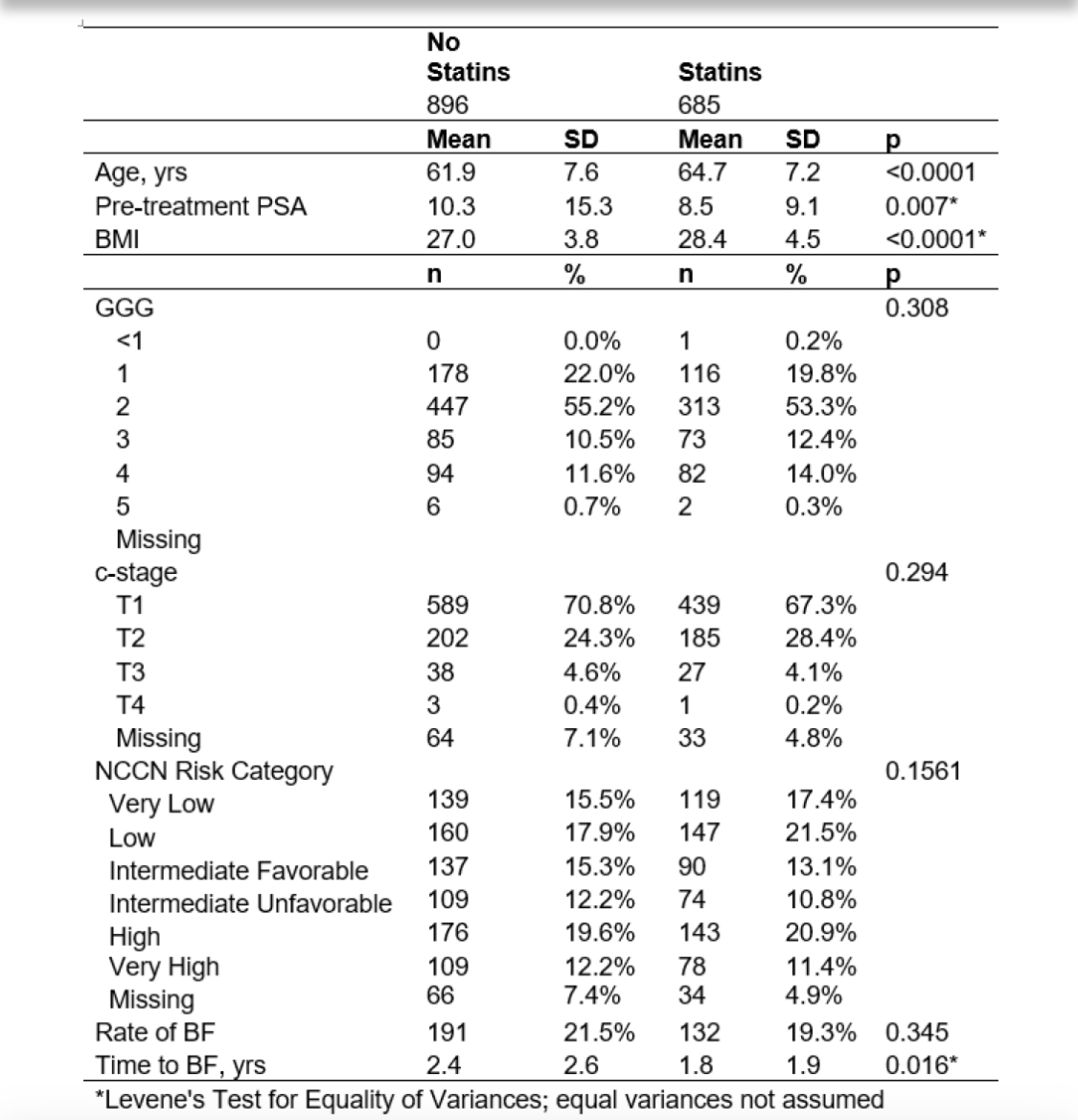
1,581 patients undergoing radical prostatectomy (RP) or radiation therapy (RT) for primary treatment of PCa between July 2007 and January 2020 were evaluated for statin use, demographic/oncologic characteristics, and biochemical outcomes.
Rate of biochemical failure (BF) was assessed overall and at 1, 3, and 5 years; time to BF was estimated with Kaplan-Meier. Logistic and linear regression were used to control for treatment modality and disease characteristics.
Results
The average age was 63.0 ± 7.5 years and median pre-treatment PSA was 6.55 (IQR 4.94). 1,473 (93.2%) and 108 (6.8%) underwent RP and RT, respectively. RP patients were younger, had lower pre-PSA, lower BMI, and lower risk disease. At 3.4 ± 2.7 years follow-up, 323 (20.4%) experienced BF.
When stratified by statin use, BF overall and within 1, 3, and 5 years were not different. Time to BF was lower in patients using statins (1.8 ± 1.9 years vs. 2.4 ± 2.6 years; p=0.016). These results persisted in multivariate analysis, wherein statin use was not associated with BF but was associated with shorter time to BF. 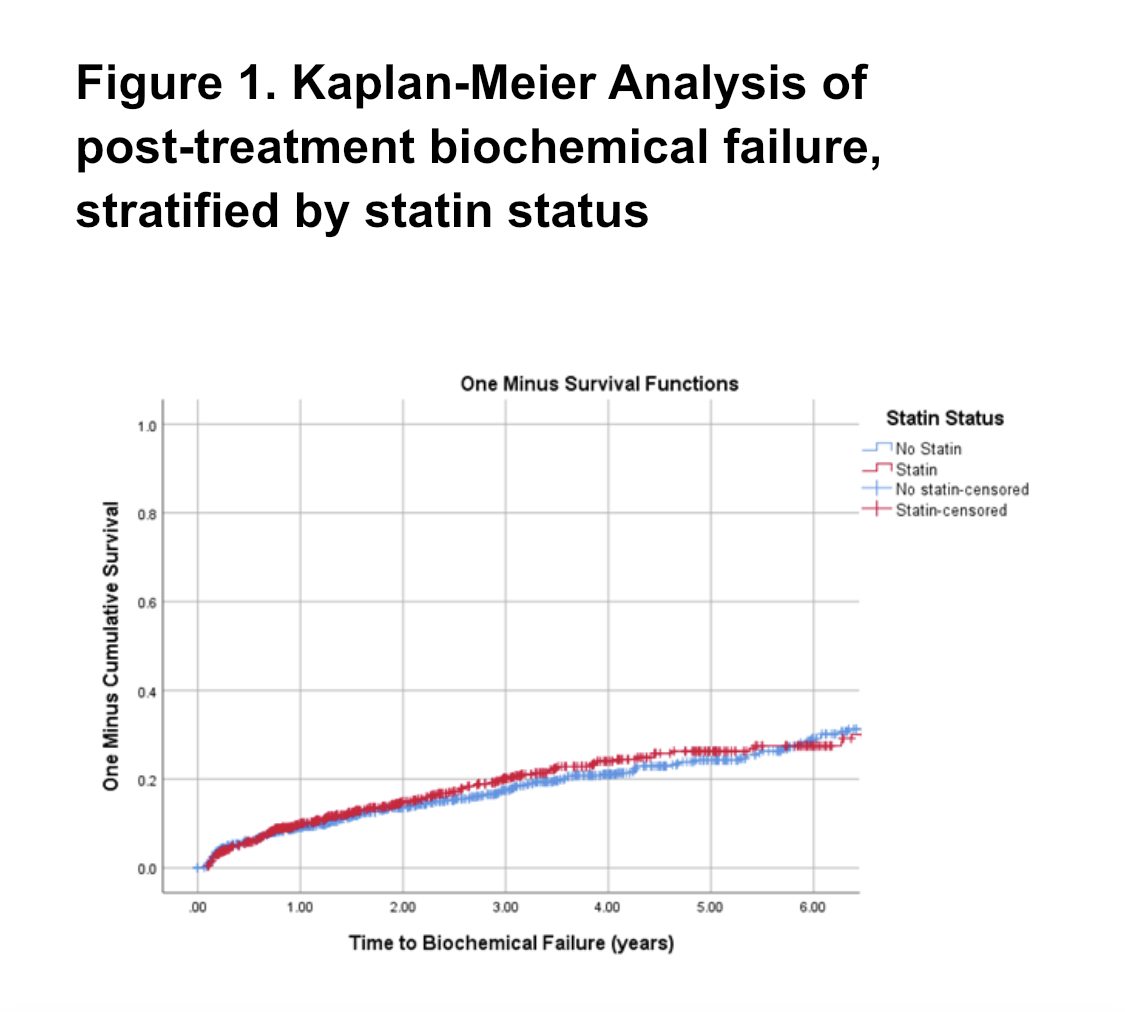
Conclusion
Overall, statin use was not associated with reduced risk of BF in RP or RT patients. However, for patients with BF, statin use was associated with a decreased time to BF. Future investigations are warranted to further elucidate impact of statin use on PCa recurrence.