Comorbidity index and LVSI for treatment selection for intermediate risk endometrial cancer patients
Janjira Petsuksiri,
Thailand
PO-1357
Abstract
Comorbidity index and LVSI for treatment selection for intermediate risk endometrial cancer patients
Authors: Janjira Petsuksiri1, Jiraporn Setakornnukul1, Aniwat Berpan1, Kullathorn Thephamongkhol1, Pittaya Dankulchai1, Atthapon Jaishuen2
1Faculty of Medicine Siriraj Hospital, Mahidol University, Radiation Oncology, Bangkok, Thailand; 2Faculty of Medicine Siriraj Hospital, Mahidol University, Obstetrics and Gynecology, Bangkok, Thailand
Show Affiliations
Hide Affiliations
Purpose or Objective
To compare treatment outcomes
between pelvic radiotherapy (PRT) versus vaginal brachytherapy (VBT) as
adjuvant treatment for intermediate-risk endometrial cancer patients.
Specifically, this study aims to provide high risk factors that increase pelvic
recurrences, requiring PRT in addition to VBT.
Material and Methods
Patients with intermediate-risk endometrial cancer
who received postoperative VBT alone or PRT with or without VBT were included. Primary endpoint was
locoregional recurrence (LRR). Secondary
endpoints were vaginal recurrence (VR), pelvic recurrence (PR), distant metastases
(DM), overall recurrence (OR), progression free survival (PFS), cancer-specific
survival (CSS), overall survival (OS) and complications. Specific
risk factors were explored to indicate the benefits of PRT over VBT alone.
Results
From 2005 - 2017, 322 patients were included for analyses. There was no difference in 5-year LRR,
VR, PR, DM, OR, CSS or OS, comparing between patients who received VBT versus PRT with or without VBT (table 1). Acute and late GI and GU toxicities were significantly higher in the PRT arm
than VBT arm (grade 1-2 acute GI: 0% vs 54.4%; GU: 3.3% vs 17.2%; late GI: 1.3% vs
12.4%; GU: 1.3% vs 8.3%, p <0.001). On
univariable and multivariable analyses, lymphovascular space invasion (LVSI) was a significant prognostic
factor for OR (HR 4.71; 1.41-15.73, p= 0.012) and CSS (HR 3.04;
1.03-8.99, p=0.045),
while high age-adjusted Charlson comorbidity index (ACCI) was independently
associated with worse non-CSS (HR 1.78; 1.38-2.29,
p<0.001)
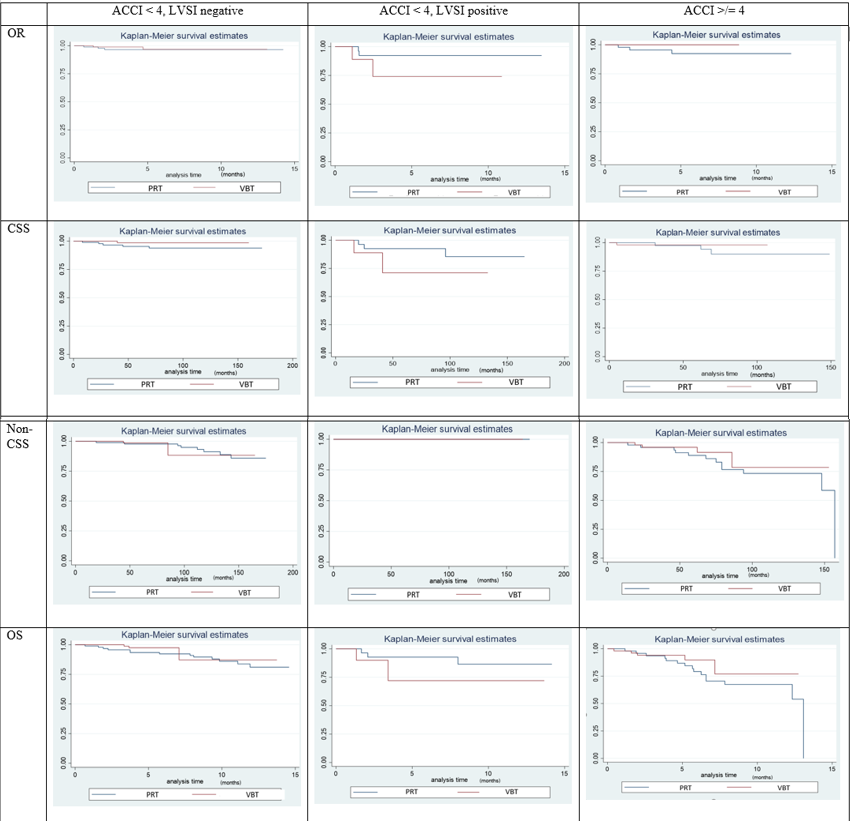
and OS (HR 1.51; 1.23-1.86, p<0.001). On specific analyses, PRT appeared to
have better oncologic outcomes specifically in patients with ACCI of less than
4 and LVSI (figure 1).
Table 1: Outcomes
stratified by treatment groups
|
5-year
|
VBT alone (n=153) % (95% CI)
|
PRT with/without VBT (n=169) % (95% CI)
|
Absolute difference % (95% CI)
|
Hazard ratio (95% CI, p-value)
|
|
LRR
|
0.8 (0.1-5.7)
|
1.9 (0.6 - 5.8)
|
-1.1
(-3.8 to 1.6)
|
0.37;
0.04 – 3.54, 0.387
|
|
VR
|
0
|
1.3 (0.3-5.1)
|
-1.3
(-5.1 to 0.3)
|
-
|
|
PR
|
0.8 (0.1-5.5)
|
0.6 (0.1-4.2)
|
0.2
(-1.8 to 2.1)
|
1.11;
0.07-17.67, 0.944
|
|
DM
|
3.0 (0.9-9.8)
|
3.4 (1.4-8.0)
|
-0.8
(-5.0 to 3.3)
|
0.73;
0.17 – 3.09, 0.674
|
|
OR
|
3.8 (1.3-10.5)
|
5.3 (2.7-10.4)
|
-2.0
(-6.7 to 2.9)
|
0.59;
0.18 – 1.96, 0.387
|
|
CSS
|
95.4
(89.0-98.1)
|
94.2
(89.1-96.4)
|
-2.3
(-7.8 to 3.2)
|
0.55;
0.19-1.56, 0.258
|
|
OS
|
95.0
(89.8-97.6)
|
91.4
(85.9-94.8)
|
-3.4
(-9.3 to 2.5)
|
0.67;
0.33 – 1.36; 0.265
|
Figure 1: Survival according to ACCI and LVSI
Conclusion
Postoperative VBT alone is
sufficient for intermediate-risk endometrial cancer. PRT could be recommended for low ACCI patients
with LVSI.