Prognostic factors in patients receiving palliative radiotherapy for female genital tract cancer
Sri Harsha Kombathula,
United Kingdom
PO-1348
Abstract
Prognostic factors in patients receiving palliative radiotherapy for female genital tract cancer
Authors: Sri Harsha Kombathula1, Anthea Cree1,2, Priya V. Joshi3, Nesrin Akturk1, Lisa H Barraclough1, Kate Haslett1, Ananya Choudhury1, Peter Hoskin1,3
1The Christie NHS Foundation Trust, Clinical Oncology, Manchester, United Kingdom; 2The Clatterbridge Cancer Centre, Clinical Oncology, Liverpool, United Kingdom; 3Mount Vernon Cancer Centre, Clinical Oncology, Northwood, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
The 5 year survival of female genital tract cancer (FGTC) is approximately 15%. In
the management of advanced female genital tract cancer (FGTC), palliative
radiotherapy plays an important role. There is little data reporting the
outcome of palliative radiotherapy in this setting and the quality of evidence
available for prognostic indicators to inform patient selection is suboptimal.
Material and Methods
Data of patients receiving palliative radiotherapy for FGTC
was collected retrospectively including patient demographics, disease and
treatment characteristics from two UK cancer centres. Overall survival was
calculated from the date of completion of radiotherapy using the Kaplan Meier
method. Descriptive statistics were used
for quantitative variables. The
association between the patient, disease and, treatment factors and the
survival after completion of radiotherapy was analysed using ANOVA with a
significance threshold of p=0.05.
Results
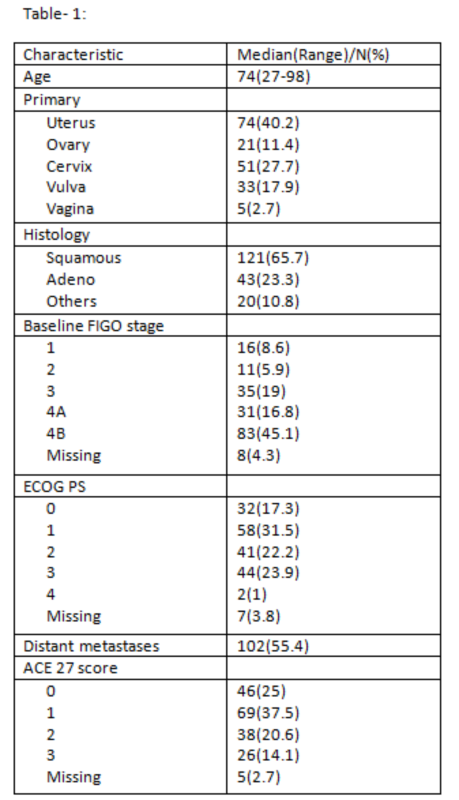
A total of 184 patients were included in the study. Table-1
shows baseline patient demographics. Of all patients, 35.3% received prior
radical treatment for FGTC and then subsequently relapsed. The radiotherapy
schedules used varied significantly and ranged from 10Gy/1# to more protracted
regimens like 50Gy/20# but the most commonly used regimen was 35Gy/15#(33.6%). The
prescribed regimens were well tolerated with only 1.7% unable to complete the planned course of palliative
radiotherapy. Most patients (40.7%) did not experience acute toxicity related
to palliative radiotherapy, however, grade 3 acute toxicity was noted in 8.1% of
the patients. After completion of palliative radiotherapy, 70.6% had a subjective
response and 34.2% went on to have further cancer-directed treatment.
The median survival after radiotherapy is 6 months and
ranged from 1 month to 6 years. Upon analysis of the prognostic factors, the absence
of distant metastases (p=0.019) and receipt of further lines of treatment (p=0.045)
were found to have a positive influence on the survival after radiotherapy. Qualitative
variables like performance status, comorbidities (ACE-27) and quantitative
variables like EQD2 of the radiotherapy schedule, number of metastases or visceral
metastases did not significantly associate with survival post palliative
radiotherapy.
Conclusion
Palliative radiotherapy to the pelvis in advanced FGTC is
well tolerated with a majority having a subjective response. Patients with
distant metastases who could not receive further lines of oncologic treatment
fared significantly poorly. With limited life expectancy in these patients, choice
of radiotherapy schedule is key when balancing symptoms and pelvic disease
control.