COMPARING MRI AND 18FDG-PET/CT AS RESPONSE EVALUATION TOOLS IN LOCALLY ADVANCED CERVICAL CANCER
MARIA ISABEL GARRIDO BOTELLA,
Spain
PO-1344
Abstract
COMPARING MRI AND 18FDG-PET/CT AS RESPONSE EVALUATION TOOLS IN LOCALLY ADVANCED CERVICAL CANCER
Authors: MARIA ISABEL GARRIDO BOTELLA1, MARTA RODRIGUEZ ROLDAN1, MACARENA TEJA UBACH1, MERCEDES GONZALEZ CANTERO1, ISABEL RODRIGUEZ RODRIGUEZ1, ELISABET GONZALEZ DEL PORTILLO1, BELEN BELINCHON OLMEDA1, ROSA MORERA1
1HOSPITAL UNIVERSITARIO LA PAZ, RADIATION ONCOLOGY, MADRID, Spain
Show Affiliations
Hide Affiliations
Purpose or Objective
Standard treatment in locally advanced cervical cancer (LACC; FIGO stage ≥IB2) is definitive concurrent chemoradiotherapy (cCRT), with external beam radiotherapy and weekly cisplatin, followed by brachytherapy (BT).
In the early assessment of tumoral response, the regression of the tumor could be a survival prognostic factor.
By this study we want to compare concordance of magnetic resonance image (MRI) and 18F-fluorodeoxyglucose positron emission tomography – computed tomography (18FDG-PET/CT) as early response evaluation tools, and to describe survival rates in the first 24 months of follow up according to early response.
Material and Methods
A retrospective observational study was performed, including patients (n=94) with LACC, treated with cCRT (treatment volume defined according to RTOG guidelines, with 3D conformed radiotherapy or volumetric modulated arc therapy with 6-MV photons, to a total dose of 45-50.4Gy, 1.8Gy per fraction 5 days a week, with dose escalation if positive pelvic nodes or extracapsular extension on paraaortic lymphadenectomy were objectified, and 2-7 cycles weekly cisplatin) followed by high dose rate BT (total dose of 26Gy, 6.5Gy per fraction, twice a week, with Iridium-192, using Ring or Fletcher applicator) between 2010-2018 in our institution.
Response to treatment was objectified 18FDG-PET/CT (n=77) performed 3 months after treatment and MRI (n=69) performed 3-6 months after treatment. Results were classified as complete (CR), partial response (PR), stable disease (SD), or disease progression (DP). We described survival rates in patients with CR, PR or SD compared to survival rates in patients with disease progression.
Results
Same result was obtained in early response assessment by MRI and 18FDG-PET/CT in 69.57% of patients (CI 57.92-79.15).
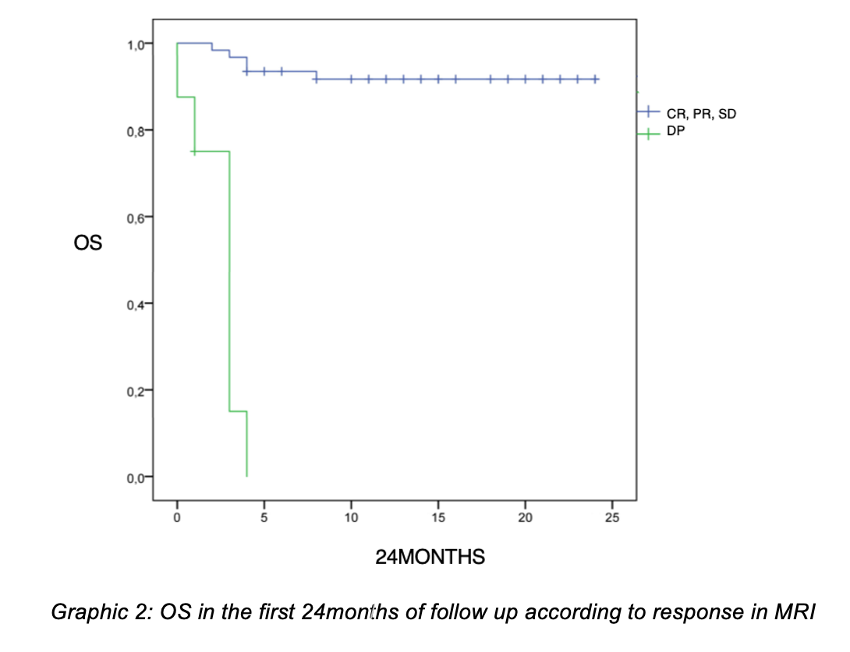
OS after 24 months of follow up in patients with response to treatment or SD objectified in early MNR was 91.8% and 12.5% in patients with DP (p<0.001). Response to treatment or stable disease in MRI affects overall survival, reducing decease risk 96.9% (p<0.001).
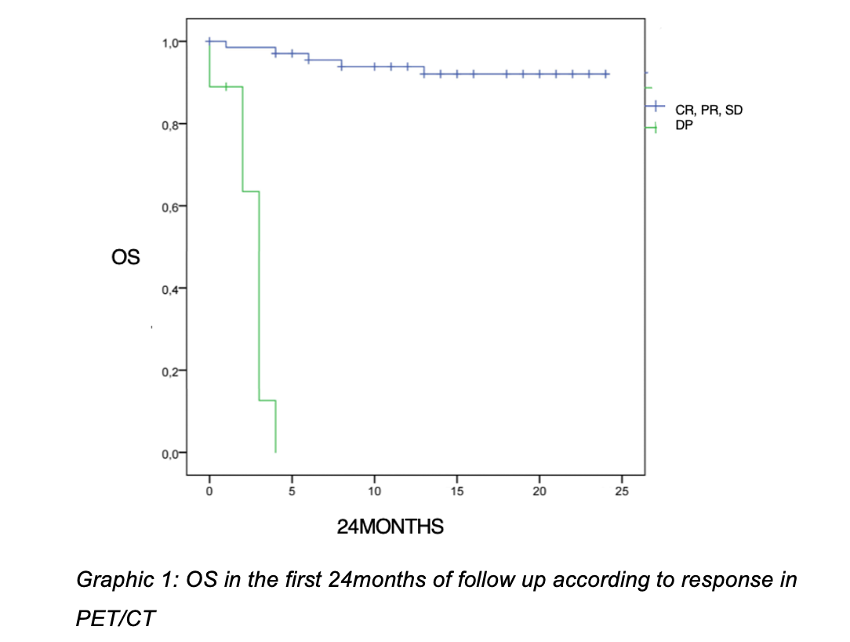
OS after 24 months of follow up in patients with response to treatment or SD objectified in early 18FDG-PET/CT was 92.6% and in patients with disease progression was 11.1% (p<0.001). Response to treatment or SD in 18FDG-PET/CT affects OS, reducing decease risk 98.6% (p<0.001).
Better survival rates were objectified according to better response in both imaging test.
Conclusion
MRI and 18FDG-PET/CT are useful tools in the evaluation of early response after treatment in locally advanced cervical cancer.
Early response assessed either by MRI or 18FDG-PET/CT is a good prognostic factor to estimate specific-cause survival in these patients.
Further investigation should be done to stablish the reliability of both techniques to stablish them as definitive prognostic tools to estimate survival rates.