Clinical outcomes of uterine body cancers treated in a tertiary cancer centre in South India
Muthulingeshkumar K,
India
PO-1335
Abstract
Clinical outcomes of uterine body cancers treated in a tertiary cancer centre in South India
Authors: Muthulingeshkumar K1, Jagadesan Pandjatcharam1, Latha Chaturvedula2, Pragna Sagar1
1Jawaharlal Institute of Postgraduate Medical Education and Research, Radiation Oncology, Pudhucherry, India; 2Jawaharlal Institute of Postgraduate Medical Education and Research, Obstetrics and Gynaecology, Pudhucherry, India
Show Affiliations
Hide Affiliations
Purpose or Objective
To
report the clinical outcomes of uterine body cancers in South Indian
population. The primary outcome of our study was overall survival (OS). The
secondary outcomes were disease free survival (DFS), patterns of recurrence,
toxicities of radiation treatment and the association of patient, disease and
treatment characteristics with survival and recurrence.
Material and Methods
Records of the patients diagnosed
as malignancy in uterus treated from January 2013 to December 2017 were retrieved after Institute
Ethics Committee approval. Demographic, surgical, histopathology and adjuvant
treatment details were retrieved. Patients of endometrial adenocarcinoma were
stratified according to ESMO-ESGO-ESTRO consensus for analysis and overall
outcomes irrespective of histology were also analyzed. For the survival analysis,
Kaplan-Meier survival estimator was used. Cox regression was used to test the
significance of association of factors with outcomes in terms of hazard ratio.
Results
178
patient records were retrieved. The median follow up of all patients was 30
months (0.5 to 81 months). The median age of the population was 55 years. Most
common histology was endometrioid type of adenocarcinoma (89%), sarcomas
comprised only 4%. 158 patients had undergone surgery, among which nodal
regions addressed for 77 patients by either pelvic lymph node dissection (PLND)
or para-aortic nodal dissection or both. Radiation therapy was delivered to 87
patients among which 72 patients received adjuvant radiation, 7 patients received preoperative radiation and 8 patients received radical radiation in view of their
medical comorbidities. The mean OS of all patients was 68 months (n=178),
median was not reached. 5-year OS was 79 %. Median survival was not reached for
stage I, 40 months for stage II, 71 months for stage III and 8 months for stage
IV. 5-year OS rates observed in low, intermediate, high- intermediate and high
risk were 91%, 88%, 75% and 81.5% respectively. The mean DFS was 65 months,
median not reached. The 5 year DFS was 76 %. The 5 year DFS rates observed were
82%, 95%, 80% and 81.5% for low, intermediate, high intermediate and high risk
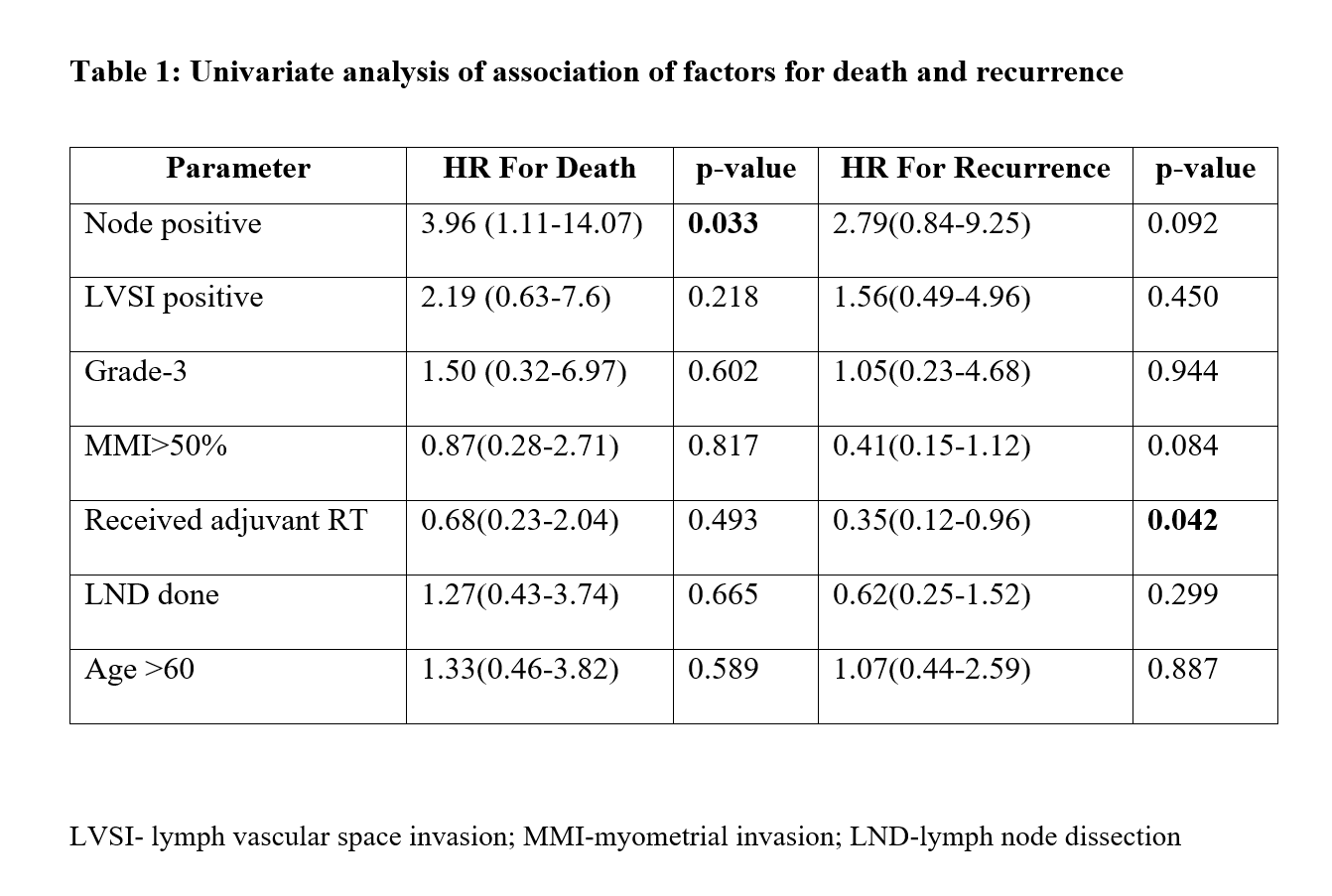
respectively. Univariate analysis using cox regression showed increase in hazard
for death in case of node positivity, HR-3.96 (p-0.033). The hazard ratio for
disease recurrence was 0.35 (p-0.042) in patients who had received adjuvant
radiation therapy. No other factors had any significant impact on death or
disease recurrence. Toxicities details were found inadequate to report.
Conclusion
The survival outcomes in terms of disease free
survival and overall survival were comparable with other Indian and Western
data reported in the published literature. Based on ESMO-ESGO-ESTRO consensus
risk stratification, we had reported better survival rates in the low and
intermediate risk groups which is also comparable with other reports from India.