CT radiomic predictors of local relapse after SBRT for lung oligometastases from colorectal cancer
PO-1315
Abstract
CT radiomic predictors of local relapse after SBRT for lung oligometastases from colorectal cancer
Authors: Martina Mori1, Roberta Tummineri2, Simone Baroni2, Michela Olivieri1, Sara Broggi1, Chiara Lucrezia Deantoni2, Paola Mangili1, Andrei Fodor2, Antonella Del Vecchio1, Claudio Antonio Fiorino1, Nadia Gisella Di Muzio2
1IRCCS San Raffaele Scientific Institute, Medical Physics, Milan, Italy; 2IRCCS San Raffaele Scientific Institute, Radiotherapy, Milan, Italy
Show Affiliations
Hide Affiliations
Purpose or Objective
Lung oligometastases (LOM) from colorectal cancer (CRC) treated with SBRT are more radioresistant than those from other cancers. The purpose of this pilot study was to assess the ability of Radiomic Features (RF) derived from pre-treatment CT images in predicting Local Progression (LP) after SBRT.
Material and Methods
Thirty-eight patients previously treated at our Institute with SBRT (40-60 Gy in 3-9 fractions, 7.5-20 Gy/fr) delivered with Helical Tomotherapy or Cyberknife (Accuray, Sunnyvale, Ca, USA) were considered. The largest LOM were delineated on pre-SBRT CT by two expert clinicians. After imageresampling (voxel size: 1x1x1 mm3) and rebinning (64 bins), 141 CT-RF were extracted from both contours according to IBSI (Image Biomarker Standardization Initiative) guidelines using the SPAARC software (Whybra et al Sci Rep 9:9649 (2019)). The selection of CT-RF robust against delineation (134/141) was performed based on ICC coefficients of the agreement between the two observers (ICC>0.80); independent CT-RF were then assessed by Spearman correlation coefficients (S). Among redundant RF the most informative ones were selected, based on the lowest p-values (<0.05) from Univariate Logistic Regression (ULR) testing the presence/absence of LP. The ability of RF in discriminating LP was finally assessed by the p-value of the Mann-Whitney test (MW) and ROC analysis.
Results
15/38 patients experienced LP with a median time to progression equal to 15 (inter-quartile range: 10-26) months; 5/141 CT-RF resulted significantly associated to LP in ULR analysis (pURL<0.05), among them, 4 RF were selected as robust and independent: Statistical_Variance (AUC=0.75, p=0.002, MW=0.009), Statistical_Range (AUC=0.72, p=0.013, MW=0.021), GLSZM_zoneSizeNonUniformity (AUC=0.70, p=0.022, MW=0.041), GLDZM_zoneDistanceEntropy (AUC=0.70, p=0.026, MW=0.044). The corresponding Box-plot of these CT-RF are shown in the Figure below according to LP status. Interestingly, Volume was not associated to LP; the correlation between the predictive CT-RF and Volume was variable (S=0.30-0.95) with the lowest value for the CT-RF showing the best discrimination power (Statistical_Variance: S=0.30). Of note, BED10 and the available clinical parameters (age, primary site, initial stage) were not found to be associated with LP except for male sex (AUC=0.66, p=0.042, MW=0.05).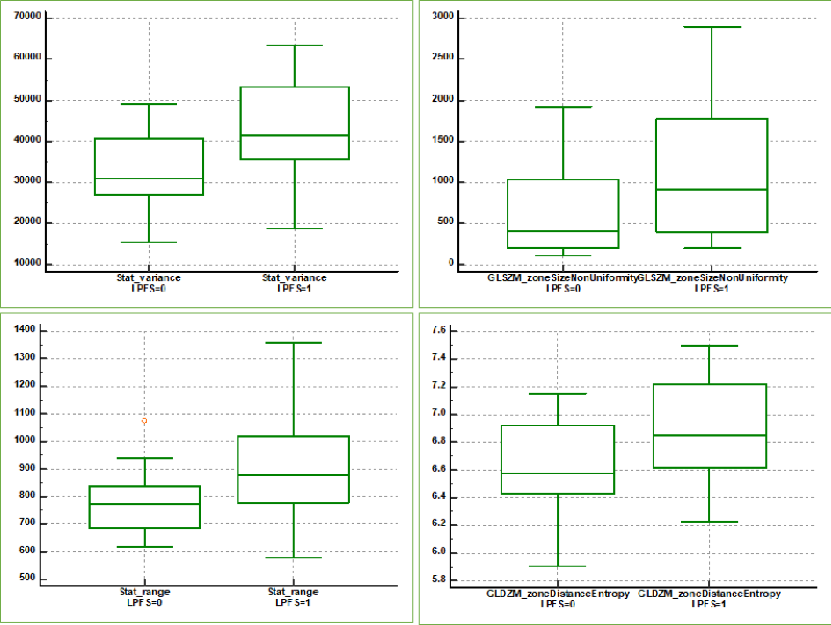
Conclusion
Despite the relatively small group of patients, some CT-RF were significantly associated with LP of CRC treated with SBRT. The heterogeneity of HU values within LOM, as expressed by their variance, was suggested to be the most promising CT-RF. Results need to be extended and replicated in larger populations.