clinical prognostic factors for esophageal cancer treated with definitive chemo-radiotherapy
PO-1294
Abstract
clinical prognostic factors for esophageal cancer treated with definitive chemo-radiotherapy
Authors: Sergio Favareto1, Cecilia Sousa1, Pedro Pinto1, Henderson Ramos1, Elson Neto1, Carolina Abrahao1, Michael Chen1, Antonio Cassio Pellizzon1, Maria Leticia Silva1, Guilherme Gondim1, Douglas Castro1, Ricardo Fogaroli1
1AC Camargo Cancer Center, Radiation Oncology, São Paulo, Brazil
Show Affiliations
Hide Affiliations
Purpose or Objective
Evaluate clinical prognostic factors for progression-free survival (PFS) and overall survival (OS) in patients with esophageal cancer treated with definitive radiotherapy (RT) and chemotherapy (CT).
Material and Methods
Clinical records of 60 patients treated from April 2011 until December 2019 with esophageal cancer considered unresectable and/or without clinical conditions for surgery, treated with definitive CRT were analyzed. All patients had upper digestive endoscopy (UDE) with positive biopsy, neck, chest and abdominal CT-scan (CT) and 18F-fluorodeoxyglucose positron-emission tomography (PET-CT). Patients were followed with physical examination, and CTs every three months in the first and second year and every 6 months from the third year of follow-up. UDE was made every three to six months after the end of the treatment or in suspicion of tumor recurrence. PET-TC was also performed in the follow-up when clinically necessary. Local and regional failure (LRF) were defined as abnormalities in the image tests within the PTV (planning target volume) and/or positive biopsy on UDE. Any other failure was defined as a distant failure (DF). PFS was defined in the record of the first tumor recurrence site and OS in the death record from the date of the start of treatment.
Results
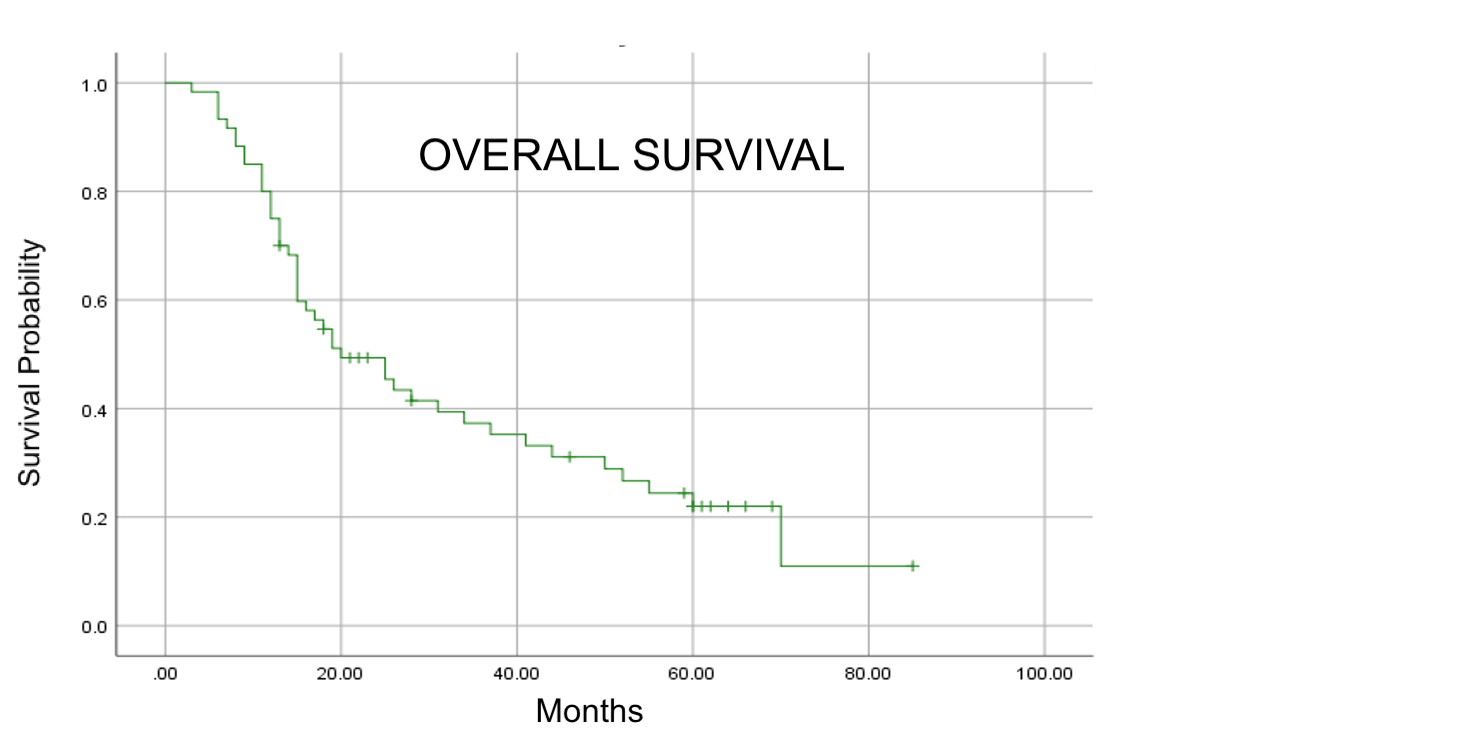
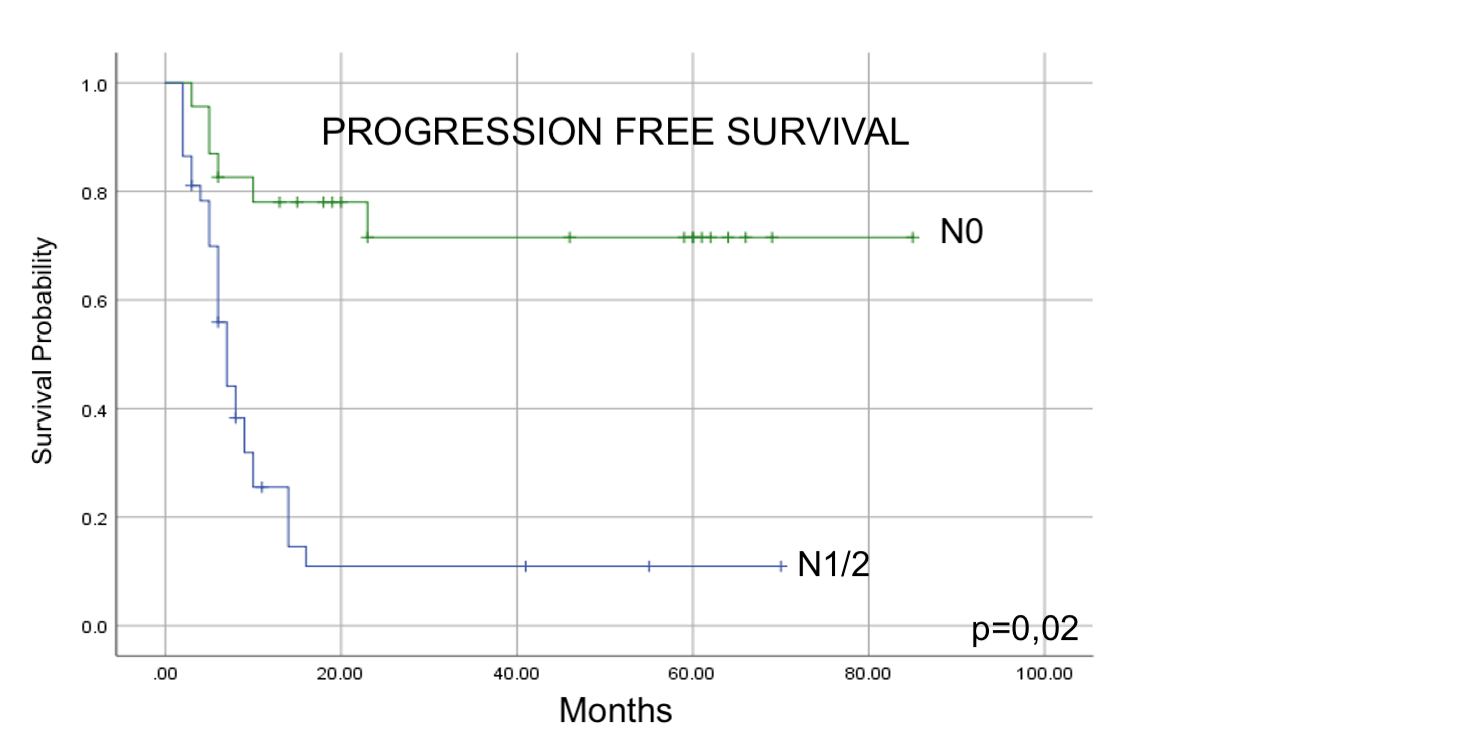
The median age of the patients was 66 years (range: 33 to 83 years) and 46 patients (76,7%) were male. Squamous cell carcinoma (SCC) was the most frequent histological type (85%). Most patients had tumors located in the mid-thoracic esophagus (53,3%) and stage III or IV (59,9%). All patients were treated using 3D (76,7%) or IMRT (23,3%). The median total dose was 50,4Gy. All patients received platinum-based CT concomitant with RT. The most common regimen used was carboplatin and paclitaxel, with a median of 5 cycles. With a median follow-up of 19 months the median PFS and OS (figure 1) was respectively 10 and 20 months. LRF and DF as the first site of failure were observed respectively in 22 (36,6%) and 26 (43,3%) patients. In the univariate analysis, tumor length lower than 2.6 cm, GTV volume lower than 28 cm3, clinical tumor stage T1 and T2, clinical node stage N0, clinical prognostic stage groups I and II and complete response to treatment, were statistically significant factors for the better PFS and OS. In the multivariate analysis, the presence of node clinical N0 was related to the better PFS (p=0.02) (figure 2).
Conclusion
The node clinical status was the most important clinical factor for PFS. Despect the technical progress observed in radiotherapy, treatments with concomitant platinum-based chemotherapy are associated with high levels of LRF and DF which considered restricts the prognosis. New strategies in systemic therapy and radiotherapy are necessary for improving outcome.