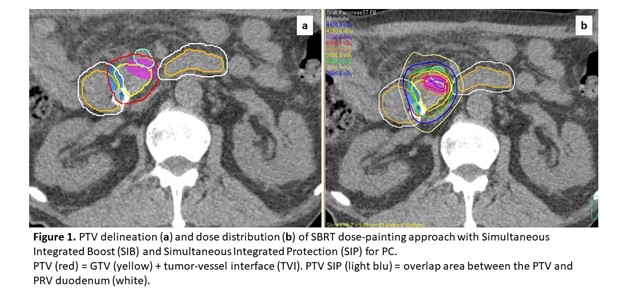
Four pilot cases have been analyzed. Dose constraint for duodenum was
set as maximum dose (0.5cc) <33Gy (5 fractions). Dose prescription on all
cases was 35Gy (5 consecutive daily fraction, 60Gy BED10), with minimal dose to
PTVs of 25Gy, and 40Gy on PTV boost (72Gy BED10). Case1: PTV volume =52cc, PTVSIP
volume =12cc, PTV boost volume =8cc. Case2: PTV volume =126cc,
PTVSIP volume =15cc, PTV boost volume =57cc. Case3: PTV volume
=107cc, PTVSIP volume =10cc, PTV volume boost=44cc; Case4: PTV volume
=109cc, PTVSIP volume =22cc, PTV boost volume =21cc.
In the four cases, the mean dose on
PTV were 35.5, 36.7, 37.1, 35Gy, the mean dose on PTVSIP were 32,
31, 33, 30Gy, the mean dose on PTVs boost were 40, 41, 39, 41Gy and the maximum
dose on PTVs boost were 41.7, 42.3, 41, 42Gy, respectively. Volumes and dose
distribution of Case1 is showed in Figure 1.