Clinical benefits of proton therapy in thymic epithelial tumors using a model-based approach
Stephanie Peeters,
The Netherlands
PO-1280
Abstract
Clinical benefits of proton therapy in thymic epithelial tumors using a model-based approach
Authors: Stephanie Peeters1, Esther Kneepkens1, Florit Marcuse2, Monique Hochstenbag2, Jos Maessen3, Dirk De Ruysscher1
1Maastro, Radiation Oncology, Maastricht, The Netherlands; 2MUMC+, Pulmonology, Maastricht, The Netherlands; 3MUMC+, Thoracic surgery, Maastricht, The Netherlands
Show Affiliations
Hide Affiliations
Purpose or Objective
Radiotherapy (RT) for thymic epithelial tumors (TET), including
thymoma and thymic carcinoma, is indicated postoperatively for advanced/aggressive
disease or incomplete resection, or as primary treatment in inoperable patients
(ESMO guideline). Proton therapy has the potential to better spare normal
tissues compared to photons, and hence reduce toxicity. The aim of this study
is to compare photon and proton plans regarding doses, normal tissue
complication probability (NTCP), and report acute toxicity in TET-patients
treated with RT at our center.
Material and Methods
All patients with TET who were referred for RT from 08.2019 until 08.2021
were included. Intensity-modulated proton therapy (IMPT) and volumetric arc photon
therapy (VMAT) plans were compared regarding mean doses to the lungs (MLD),
heart (MHD) and esophagus (MED) (using paired t-test), and normal tissue
complication probability (NTCP) with endpoints radiation pneumonitis1,
cardiac toxicity2 and acute dysphagia3. In The
Netherlands, patients are selected for IMPT if the NTCP is significantly lower,
by consensus i.e. ≥10% for radiation pneumonitis or acute dysphagia, or ≥2% lower
for cardiac toxicity4. Maximal acute toxicity for dermatitis and dysphagia according to
CTCAE is reported. VMAT plans consisted typically of 2-3 partial 6MV arcs in
the anterior region, and the dose was prescribed to the PTV. IMPT plans were
typically administered with 3 or 4 anterior and anterior oblique beams going
from 300° to 50°; robust optimization was used.
Results
Thirteen TET patients had a VMAT-IMPT planning comparison. Patient
characteristics are shown in Table 1.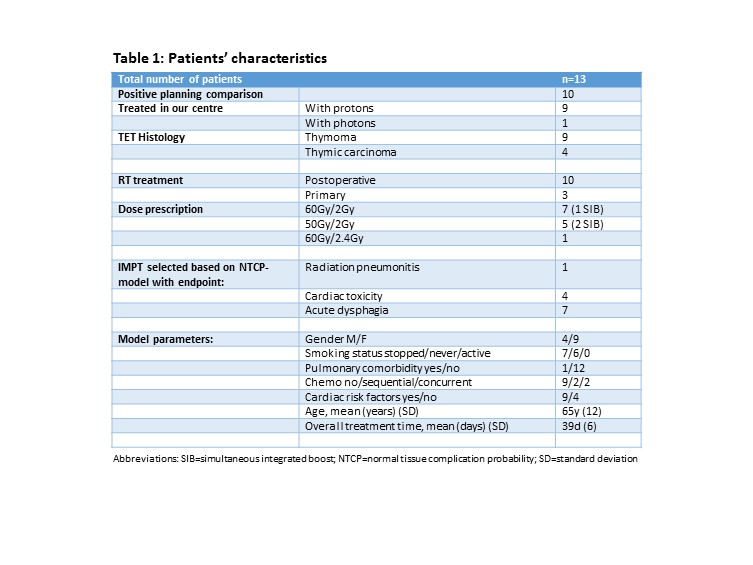
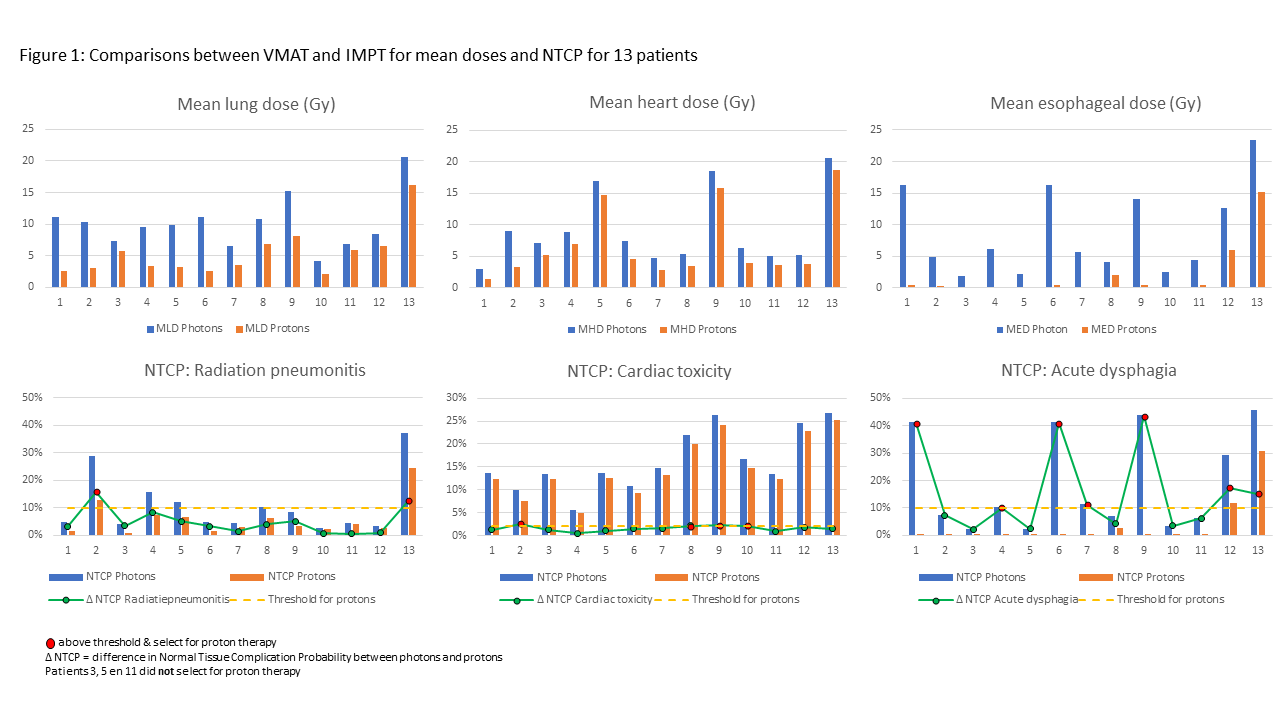
The average MLD decreased from 10.1Gy
(SD4.2) with VMAT to 5.4Gy (SD3.8) with IMPT (p<0.0001). The average MHD was
9.1Gy (SD5.8) with VMAT and 6.8Gy (SD5.7) with IMPT (p<0.0001). Finally, the
average MED diminished from 8.8Gy (SD6.9) to 2.0Gy (SD4.3) with IMPT (p<0.0001).
Average NTCP-values for radiation pneumonitis, cardiac toxicity and dysphagia
all decreased with IMPT compared to VMAT from 10.9% to 5.9%, from 16.3% to
11.5% and from 19.4% to 3.6%, respectively. Average difference in NTCP was 5.1%
(range 0.6%-15.9%) for radiation
pneumonitis, 1.5% (0.5%-2.5%) for cardiac toxicity and 18% (2.2%-43.4%) for
dysphagia. Ten patients (77%) had a significantly lower NTCP with IMPT for at
least one of the 3 endpoints (Fig.1); 9 of these were treated with IMPT at our
centre. Of the remaining 3 patients, one was treated at our centre with VMAT,
and this was the only patient developing dysphagia grade 1; all other had no
dysphagia. Dermatitis grade 0, 1 and 2 was seen in 2, 5 and 3 patients
respectively.
Conclusion
IMPT significantly reduced MLD, MHD and MED in all patients
compared with VMAT, resulting in a significant reduction of NTCP for at least one
endpoint in 77% of patients.
(1) Appelt et
al. Acta Oncol 2014;53:605-612.
(2) Darby et
al. NEJM 2013;14;368:987-998
(3) Wijsman
et al. R&O 2015;117:49-54.
(4)
www.nvro.nl