SCORE/SCORE2-OP cardiovascular risk and lung stereotactic body radiation therapy
Maria Rodriguez Pla ,
Spain
PO-1264
Abstract
SCORE/SCORE2-OP cardiovascular risk and lung stereotactic body radiation therapy
Authors: Maria Rodriguez Pla1, Ana Aliaga Chueca1, Miguel Soler Rodríguez1, Raquel García Gómez1, Esther Jordá Sorolla1, Maria Maroñas Martín1, Diego Dualde Beltrán1, Eduardo Ferrer Albiach1
1Hospital Clínico Universitario de Valencia, Radiation Oncology, Valencia, Spain
Show Affiliations
Hide Affiliations
Purpose or Objective
Stereotactic body radiation therapy (SBRT) is a therapeutic option in older patients or those with comorbidities presenting central lung lesions. Most of these patients have multiple cardiovascular risk factors. This work analyzes whether the SCORE and SCORE2-OP (Older Persons) can be a useful tool to predict a worse prognosis in patients undergoing SBRT for central and ultracentral lesions. Central lesions are more likely to receive higher heart doses than peripheral lesions. SCORE and SCORE2-OP are validated scales to assess the estimated 10-year cardiovascular risk.
Material and Methods
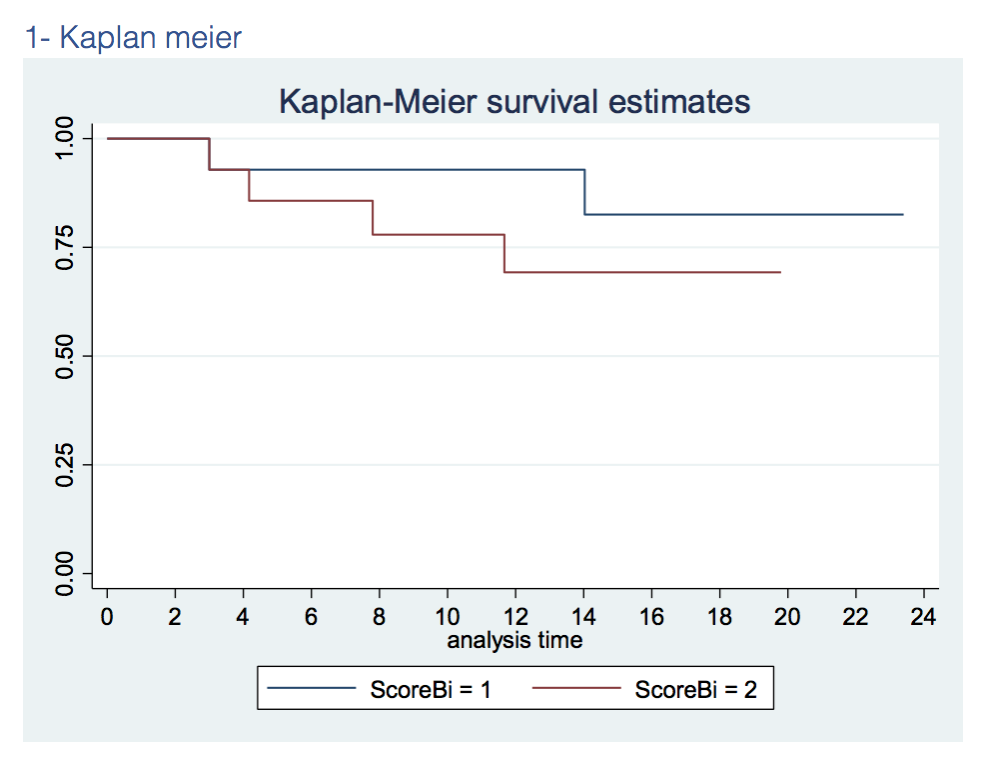
From Abril'18 to December'20, 28 patients with central lesions were radically treated with SBRT. Central lung lesions were defined according to RTOG 0813 criteria. Immobilization systems used were abdominal compressor and vacuum cushion or thorax/head-and-shoulders mask. ITV was defined by 4D RPM-Varian™.PTV was obtained by a 5mm uniform expansion of the ITV. We retrospectively reported all baseline cardiovascular risk factors and calculated their individual cardiovascular risk according to SCORE (patients with < 65y) or SCORE2-OP (patients with >65y). Kaplan-Meier survival was calculated to estimate overall survival according to SCORE / SCORE2-OP. We reported cardiac toxicity based on CTCAE v5.0. UK consensus constraints were applied.
Results
10 patients with early-stage non-small cell lung cancer, 5 non-biopsed lesions and 14 central and ultra-central lung metastases were analysed. 21 were central and 4 ultra-central lesions. Mean follow-up was 16 months (3-33). Two regimens were used: 750cGy in 8 fractions or 1000-1100cGy in 5 fractions. Mean age was 70y (52-89). Mean GTV/PTV size was 26/57.6cc (0.8-100/6.1-219). Local control was 96% at 12 months.
Patients were classified into 2 groups according to individual SCORE / SCORE-OP risk results: 10-year cardiovascular risk < 15% (group 1) or ≥ 15% (group 2). Estimated overall survival was 93% and 70% at 12 months in group 1 and 2 respectively (figure 1).
No > G3 cardiac toxicities were found.
Conclusion
VMAT based ablative radiotherapy achieves good control rates and a favourable toxicity profile. Impact on overall survival depends on a careful patient selection. SCORE and SCORE2-OP could be useful tools to better select patients. Longer follow-up and a larger sample size is needed to support this finding. We are performing one at our center.