Is SBRT an effective treatment in metastatic lung cancer with oligoprogressive disease?
PO-1261
Abstract
Is SBRT an effective treatment in metastatic lung cancer with oligoprogressive disease?
Authors: Michele Aquilano1, Mauro Loi2, Lorenzo Livi3, Joost Nuyttens4
1University of Florence, Department of Biomedical, Experimental and Clinical Sciences "Mario Serio" University of Florence, Florence, Italy; 2Azienda Ospedaliero-Universitaria Careggi, Department of Radiation Oncology , Florence, Italy; 3University of Florence, Department of Biomedical, Experimental and Clinical Sciences "Mario Serio" , Florence, Italy; 4Erasmus MC Cancer Institute, Department of Radiation Oncology, Rotterdam, The Netherlands
Show Affiliations
Hide Affiliations
Purpose or Objective
Oligoprogression (OPD) is
defined as a disease’ state where limited progression (1-3 metastases) is observed
in patients undergoing systemic treatment. Local treatment of OPD may enable to
postpone systemic therapy switch, in particular in patients undergoing novel
targeted or immune therapies. In this study we investigated the outcome after
stereotactic body radiotherapy (SBRT) in patients with metastatic lung cancer treated
with chemo-immunotherapy who were diagnosed with oligoprogression.
Material and Methods
Thirty-seven patients, 21
female and 16 male, with metastatic lung cancer and diagnosis of
oligoprogression were included and were treated with Cyberknife and Linac SBRT
between June 2015 and August 2021. SBRT was delivered to lung (n=18),
mediastinal node (n=8), bone (n=5), adrenal gland (n=5) and kidney (n=1). Dose
regimens consisted of 30-51 Gy in 3 fractions, 30-55 Gy in 5 fractions, 52.5 Gy
in 7 fractions and 44-56 Gy in 8 fractions, resulting in a median BED of 115.5
(range 48-138) Gy10. Dose was expressed as Biological Effective Dose
for α/β=10 (BED10). Kaplan-Meyer method was used to calculate Overall
Survival (OS), Local Control (LC) and Disease Progression-free Survival (DPFS)
from the start date of SBRT to event.
Results
After a median follow up of 20
months (range 1-48), median overall survival
was 26 months (figure 1), and
median DPFS was 6 months. LC was 82% at 1 year and 74% at 2 years. Median age
was 66 years (range 25–82). All patients were treated with systemic treatment
before the start of the SBRT: 9 chemotherapy (CT) alone (24%), 14 CT plus
immunotherapy (IT) or plus Tyrosin kinase inhibitors (TKI) (38%) and 14 IT/TKI
alone (38%). At univariate analysis, age, type of systemic treatment, and
number of chemotherapy lines were not significant prognostic factors for overall
survival. 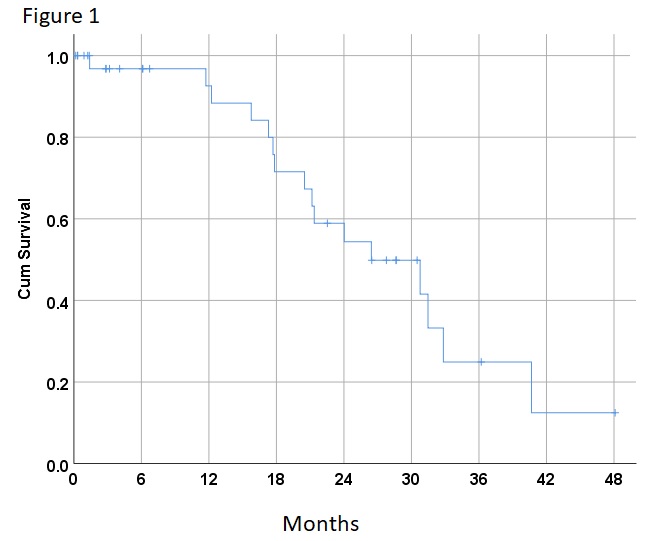
Conclusion
SBRT in lung cancer patients for
oligoprogression resulted in a long median overall survival of 26 months. Local control at 1 year was 82%. The median DFS was 6
months as other metastases grow slowely. SBRT could be a valid alternative to
postpone the change of chemotherapy and/or immunotherapy. More research is
needed to address the gain of the SBRT in patients with oligoprogressive
disease.