Of the 883 patients included in the study, 311 (35.2%)
received mastectomy, 265 (30%) received BCS+RT and 307 (34.8%) received BCS. The
median age was 56 years old (range, 18–87). Prognostic score calculation was
available for 859 patients as follows: 289 (33.6%) scored <2 points and 570
(64.6%) scored ≥2 points. Resection margin status was as follows: positive
(R1) in 36 (4.1%), close (<2 mm) in 144 (16.3%), ≥2 mm in 657 (74.1%), and
unknown margin status in 46 (5.2%) patients. At the median follow-up of 14.8
years (range of 0.1–27), 37 (4.2%), 45 (5.1%), 5 (0.5%), and 18 (2%) patients
experienced non-invasive ipsilateral breast tumor recurrence (IBTR), invasive IBTR,
regional recurrence and distant relapse, respectively, and 151 (17.1%) patients
died. The 15-year LRR were 3.6%, 10.6% and 15% for the mastectomy, BCS+RT and
BCS groups, respectively. The corresponding 15-year
iRFS rates were 94%, 94% and 77% (p<0.001), respectively (Figure 1).
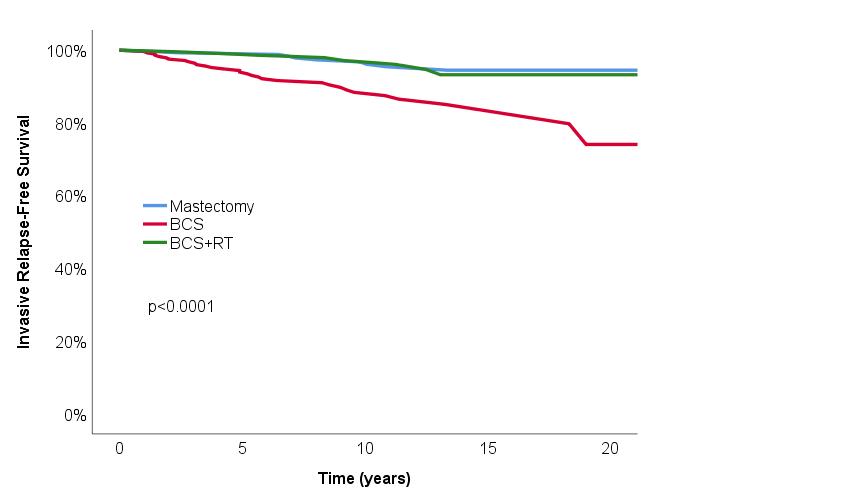
Compared to mastectomy and BCS+RT
groups, BCS group had more invasive IBTR (2.3% and 2.6% versus 10.1%; p<0.001).
There were less non-invasive IBTR in the mastectomy group compared to BCS+RT or
BCS groups (0.6% versus 7.5% and 4.9%; p>0.001). Compared to positive
resection margins (R1), negative resection margins (either <2 mm or ≥2
mm), were associated with improved iRFS (Hazard Ratio (HR) 0.75, 95% confidence
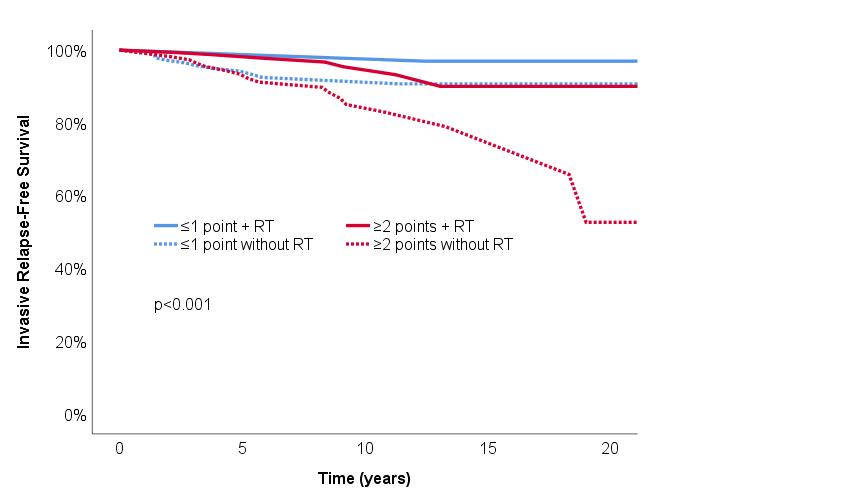
intervals (CI) 0.61–0.92; p=0.010). Among patients treated with BCS (n=572),
not-receiving postoperative RT (HR 4.06, 95 % CI 1.83–9.04; p<0.001) and a higher
patient prognostic score (≥2 points; HR 2.33, 95% CI 1.15–4.72; p=0.018) were both associated
with worse iRFS (Figure 2).