LONG TERM TOXICITY OF OARS AFTER ADJUVANT RADIOTHERAPY IN BREAST CANCER PN1 WITH OR WITHOUT ALND.
MARIA DOLORES DE LAS PEÑAS CABRERA,
Spain
PO-1199
Abstract
LONG TERM TOXICITY OF OARS AFTER ADJUVANT RADIOTHERAPY IN BREAST CANCER PN1 WITH OR WITHOUT ALND.
Authors: MARIA DOLORES DE LAS PEÑAS CABRERA1, STEPHANYIE PAYANO HERNANDEZ1, PILAR SAMPER OTS1, ENRIQUE AMAYA ESCOBAR1, JOSE ZAPATERO ORTUÑO1
1UNIVERSITY HOSPITAL REY JUAN CARLOS, ONCOLOGY RADIATION, MADRID, Spain
Show Affiliations
Hide Affiliations
Purpose or Objective
In
a previous study (ESTRO Turin 2018), we evaluated the influence of regional
nodal irradiation axillary level I-IV vs level III-IV on long term toxicity of
the OARS in patients with breast cancer, SNB positive to either 1 or 2 nodes
and SNB alone or ALND. We reported that modality
of primary axillary treatment in these patients did not influence the dosimetry
of the risk organs except for mean dose thyroid and average contralateral
breast. That showed: Dmean thyroid: 24.35±13.04 in group SNB vs 16.43±7.95 in
ALND, p=0.007. Dmean contralateral breast: 2.292±1.31 vs 2.08±1.57, p=0.03. In
the multivariate analysis, only radiation therapy modality and maximal
radiation dose were significantly associated with this parameter. The aim of
the present study was to evaluate long term toxicity of these OARS, specially focusing
on thyroid function and the presence of radiation-induced second tumors.
Material and Methods
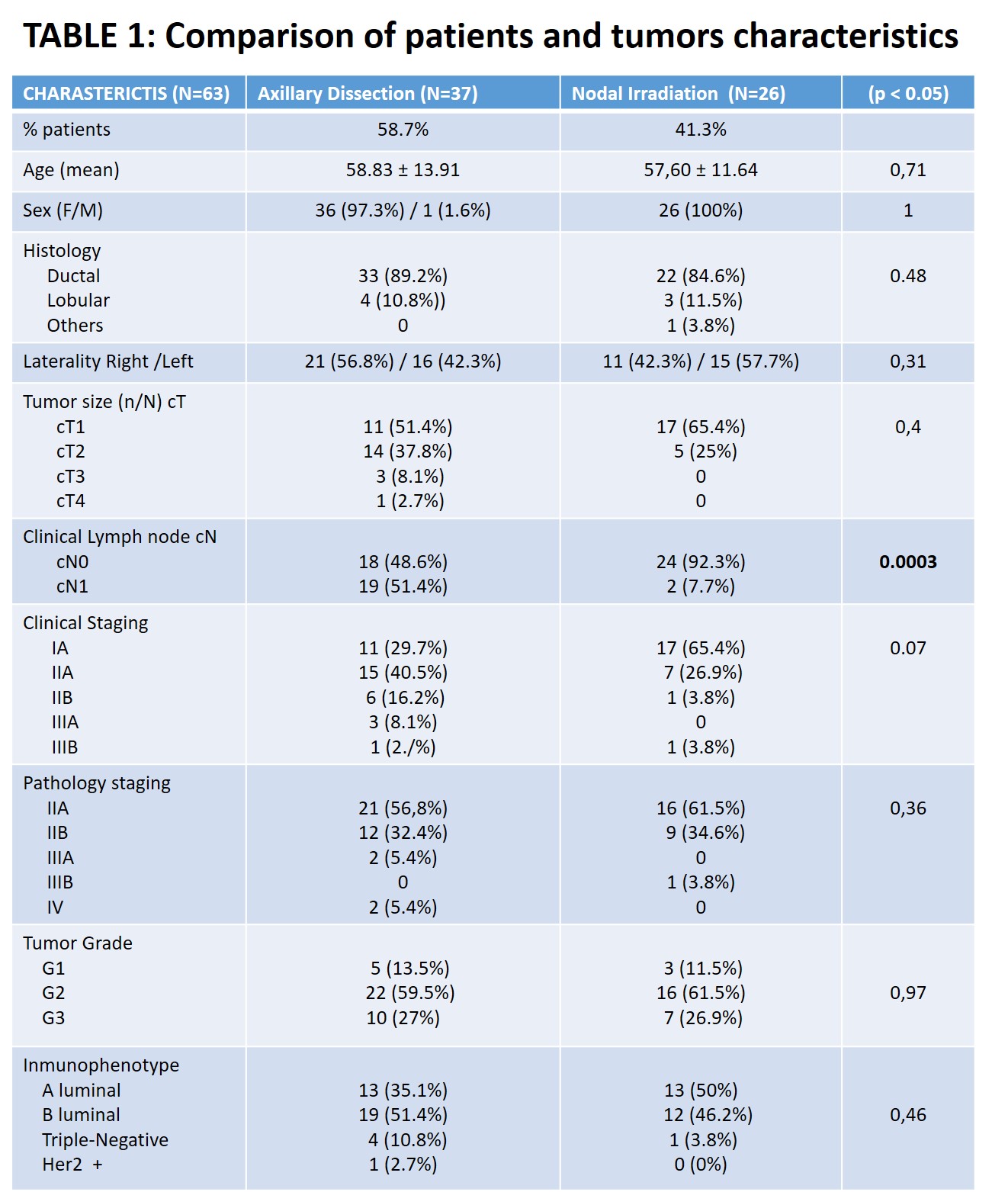
Between
October 2012 to September 2017, 63 women with cT1-T2 cN0 breast cancer that
after pathological staging were pN1 (only 1 or 2 affected nodes), were treated
by adjuvant radiotherapy. They were allocated into two groups: 26 (41.6%) of
them were staged by SNB and irradiated axillary levels I-IV and 37 (58.7%) were
staged by ALND only levels III-IV were irradiated. We followed up these
patients until September 2021. Age,
histology, laterality, cTNM, pTNM, stages and immunohistochemistry, were
similar in both groups (Table I). We also recorded TSH, thyroid hormones and
the presence of radiation-induced second tumors. Comparisons were done by using
chi squared, Student’s t test. Multiple
lineal regression was used when several variables showed significance in the
univariate analysis. Significance level was set at 95% (p < 0.05).
Results
Time of follow up was 72,72±21,23 months. Breast
late toxicity accordingly to both medical and patient criteria, was similar in
both groups 7,4% Vs. 16,7% p =0.44, All cases of lymphedema (n = 6) were present in the group ALND (0% vs.
16,7%; p=0.03). There were slightly more cases of abnormal thyroid function in
women with SNB than in patients with ALND 23,8% Vs. 5,9%, p = 0.09. There were
more cases of history of thyroid disease in this group (18,5% Vs. 2,8%), p =
0.07. Dmean thyroid was similar in patient
with and without history of thyroid disease (19,7±11,35
Vs. 19,56 ± 3,41) (p = 0,98). Thyroid mean dose was also
similar in women with and without further thyroid function abnormality (21,23±2,55
Vs 18,32±9,98; (p=0,14). There were no cases of
second breast cancer on the contralateral breast. There were only two deaths
due to lung metastases. The rate of breast-cancer specific survival was 96,8%. There were no
differences in the rate of radiation-induced second tumors 7,4% Vs. 8,3%) p=0,99.
Conclusion
The majority of patients survived after
6 years. The differences in Dmean thyroid did not influence in thyroid
function. The increased Dmean contralateral breast, was not associated with radiation-induced second tumors on this location.