Treatment planning for thermotherapy as adjuvant strategy to breast cancer preoperative radiotherapy
Sergio Curto,
The Netherlands
PO-1192
Abstract
Treatment planning for thermotherapy as adjuvant strategy to breast cancer preoperative radiotherapy
Authors: Sergio Curto1, Jannis Androulakis1, Melanie N.D. Machielse1, Kemal Sumser1, Margarethus M. Paulides2, Martine Franckena1, Linetta Koppert3, Agnes Jager4, Gerard C. Van Rhoon1
1Erasmus MC, Radiotherapy, Rotterdam, The Netherlands; 2Eindhoven University of Technology, Electrical Engineering, Eindhoven, The Netherlands; 3Erasmus MC, Surgery, Rotterdam, The Netherlands; 4Erasmus MC, Medical Oncology, Rotterdam, The Netherlands
Show Affiliations
Hide Affiliations
Purpose or Objective
Randomized clinical studies have shown the benefit of adding thermotherapy, increasing tumor temperature up to 40-44°C, as a sensitizing agent for radiotherapy and chemotherapy. Thermotherapy treatment planning (TTP) has proved to be a valuable tool in the treatment decision making and treatment implementation [Kok, 2021, Int. J. Hyperthermia 1;38(1)]. Accurate patient representative computational models are essential for the TTP process. However, patient representative models for the treatment of tumours in the intact breast have not yet been extensively investigated. The objective of this work is to investigate the feasibility of performing TTP as an adjuvant strategy to preoperative radiotherapy or neo-adjuvant chemotherapy considering wide variation of breast and tumor characteristics.
Material and Methods
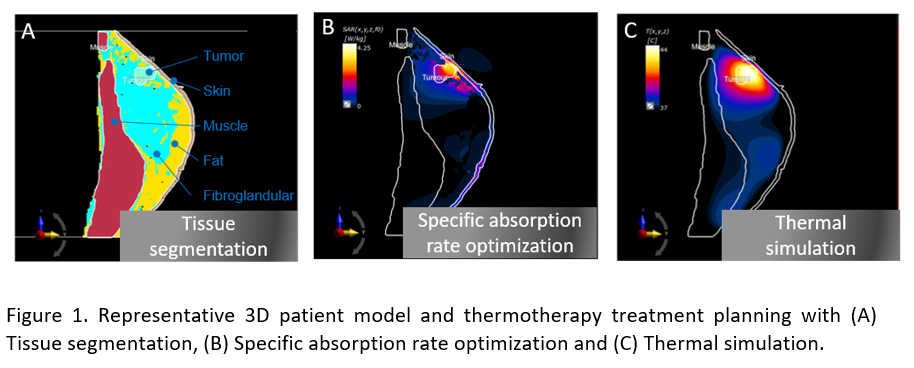
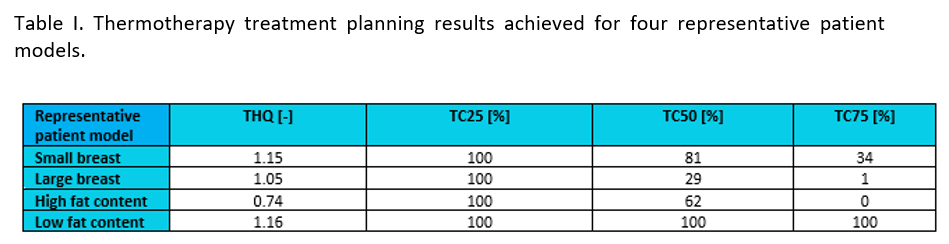
MR images of 25 invasive breast cancer patients treated in Erasmus MC were evaluated. Tissues were segmented and 3D breast patient models were generated. Variability in terms of breast volume, fat content, and tumor volume was evaluated using the generated models. A generic thermotherapy applicator consisting on 12 half-wavelength dipole antennas distributed over two rings was generated. Specific absorption rate (SAR) based TTP was performed on four models representative of small breast volume, large breast volume, high fat content and low fat content patients. Target-Hotspot-Quotient (THQ) and target coverage (TC) by the 25% (TC25), 50% (TC50) and 75% (TC75) normalized SAR contour were evaluated.
Results
Different tissues were not clearly identifiable in the MR images of three patients. This resulted in 22 patients eligible for model generation. Figure 1 shows an example of a generated breast model, SAR and thermal distribution. The generated repository contains models with a large range of breast volume (154.1-1336.5 ml), fat content (30.48-62.64 %) and tumor volume (1.44 – 39.26 ml). The THQ and TC obtained in the evaluated four representative patient models (Table I) show the feasibility of performing TTP and indicate the feasibility of good quality thermotherapy in all cases (THQ≥0.74,TC25=100%).
Conclusion
This works shows the feasibility of performing thermotherapy treatment planning in conjunction with preoperative radiotherapy. Additionally, we have generated the largest repository of patient derived breast models. This repository provides a unique platform to advance the field of intact breast thermotherapy by facilitating an objective comparison of the heating quality for different thermotherapy devices using the same set of patient derived models.