Impact of radiation techniques on hematological toxicity during craniospinal irradiation
PO-1166
Abstract
Impact of radiation techniques on hematological toxicity during craniospinal irradiation
Authors: Renu Madan1, Sureka Dhayalan1, Arun S Oinam1, Parsee Tomar1, Narendra Kumar1, Shikha Goyal1, Divya Khosla1, Kannan Periasamy1, Sushanta K Sahoo2, Chirag K Ahuja3, Debajyoti Chatterjee1
1Postgraduate Institute of Medical Education and Research, Radiotherapy and Oncology, Chandigarh, India; 2Postgraduate Institute of Medical Education and Research, Neurosurgery, Chandigarh, India; 3Postgraduate Institute of Medical Education and Research, Radiodiagnosis and Imaging, Chandigarh, India
Show Affiliations
Hide Affiliations
Purpose or Objective
Craniospinal
irradiation (CSI) is an integral component of multimodality management in
medulloblastoma (MB). Hematological toxicity is one of the commonest toxicity
observed during CSI leading to treatment breaks and increased overall treatment
time. Arc based RT techniques i.e. VMAT expose large volume of normal tissue to
low RT dose, which might increase the risk of bone marrow toxicity. The aim of
the current study is to compare the incidence of hematological toxicity in
3DCRT and VMAT technique.
Material and Methods
The study was conducted in the department of
radiotherapy and oncology, over a period of 18 months. MB patients who received
CSI during the said period were analysed.
All patients were treated in the supine position on a 6 or 15 MV linac. 3DCRT was the most commonly employed technique.
VMAT was used only if homogeneity or dosimetric constraints were not achieved. In 3DCRT technique, 2 lateral
fields were used for cranial field, matched to the spinal field by collimation
and couch rotation. VMAT was planned by 4-6 full arcs using 2-3 isocentres. Complete
blood counts were checked twice weekly during CSI. Details of patients
experiencing toxicity and treatment gap were documented in Microsoft Excel sheet. SPSS v 23 was used
for statistical analysis.
Results
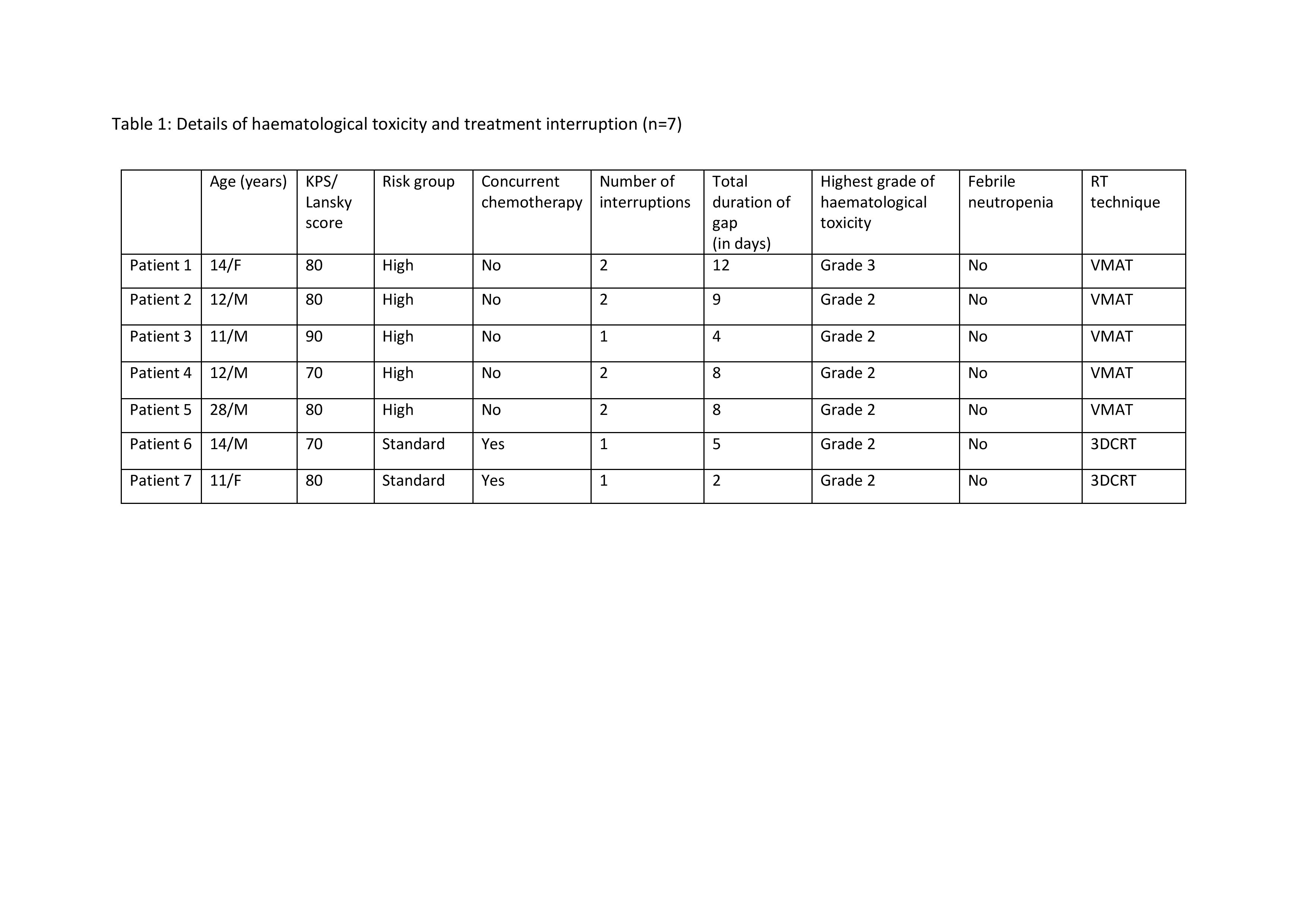
 A total of 20 patients were available for
analysis (median age 15 years). Out of this, 13 and 7 patients were treated with
3DCRT and VMAT respectively. Seven patients experienced treatment interruption due
to hematological
toxicity. Details of hematological toxicity and treatment
interruption is shown in Table 1. In VMAT group, 5 out
of 7 (71.4%) patients had at-least grade 2 hematological toxicity as compared
to only 2 out of 13 (15.4%) patients in 3DCRT group. Majority of the patients
experiencing hematological toxicities were below 14 years of age. Most of the
treatment interruptions were started in the 2nd week of CSI. The incidence
of hematological toxicity was significantly associated with bone marrow volume
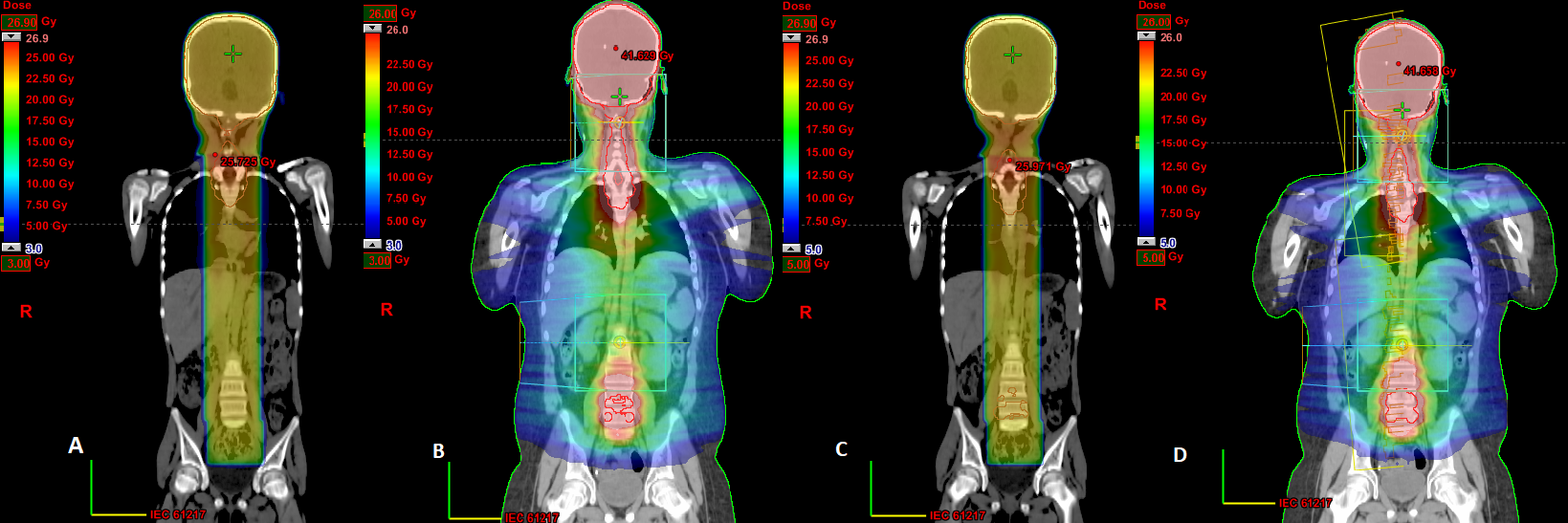
receiving low dose radiation, particularly 3 and 5 Gy (p-0.04). Figure 1 is showing dose colour wash of bone
marrow volume receiving (A) 3 Gy in 3DCRT group; (B) 3 Gy in VMAT group (C) 5
Gy in 3DCRT group and (D) 5 Gy in VMAT group. No significant association of hematological
toxicity was found with the age or baseline blood counts.
A total of 20 patients were available for
analysis (median age 15 years). Out of this, 13 and 7 patients were treated with
3DCRT and VMAT respectively. Seven patients experienced treatment interruption due
to hematological
toxicity. Details of hematological toxicity and treatment
interruption is shown in Table 1. In VMAT group, 5 out
of 7 (71.4%) patients had at-least grade 2 hematological toxicity as compared
to only 2 out of 13 (15.4%) patients in 3DCRT group. Majority of the patients
experiencing hematological toxicities were below 14 years of age. Most of the
treatment interruptions were started in the 2nd week of CSI. The incidence
of hematological toxicity was significantly associated with bone marrow volume
receiving low dose radiation, particularly 3 and 5 Gy (p-0.04). Figure 1 is showing dose colour wash of bone
marrow volume receiving (A) 3 Gy in 3DCRT group; (B) 3 Gy in VMAT group (C) 5
Gy in 3DCRT group and (D) 5 Gy in VMAT group. No significant association of hematological
toxicity was found with the age or baseline blood counts.
Conclusion
There is no substantial evidence to suggest excess
bone marrow suppression in medulloblastoma patients treated by VMAT as compared
to 3DCRT. Higher incidence of hematological toxicity in the index study, in the
VMAT group, can be explained by the high bone marrow volume exposing to low
dose radiation. Though the results from our study cannot be generalized due to small
sample size and selection bias, VMAT should be used carefully after considering
bone marrow sparing in the treatment plan optimization to reduce the incidence
and severity of hematological toxicity.