Impact of SRS to melanoma brain metastases associated with immunotherapy on OS: real-world evidence
PO-1151
Abstract
Impact of SRS to melanoma brain metastases associated with immunotherapy on OS: real-world evidence
Authors: Douglas Castro1, Carlos Henrique Teixeira2, Guilherme Gondim1, Patrícia Aguilar1, Marcos André Costa2, Thiago William Jorge2, Rodrigo Hanriot1
1Hospital Alemão Oswaldo Cruz, Radiation Oncology, São Paulo, Brazil; 2Hospital Alemão Oswaldo Cruz, Clinical Oncology, São Paulo, Brazil
Show Affiliations
Hide Affiliations
Purpose or Objective
Immunotherapy
with combined nivolumab and ipilimumab (CNI) is active in patients with
asymptomatic melanoma brain metastases (MBM), providing a significant and
durable intracranial response. Just as the treatment paradigms of MBM evolved
over the last decade, overall survival (OS) also improved based both on local and
systemic therapies. In this context, we evaluated the impact of cranial
stereotactic radiotherapy (SRT) on OS of MBM patients treated with CNI in a
contemporary and real-world setting.
Material and Methods
The study was performed by using TriNetX, a
global health network that provided a de-identified dataset of electronic
medical records from approximately 68 million patients in 49 large Healthcare
Organizations (HCO). We queried for patients with the terms: secondary
malignant neoplasm of brain and malignant melanoma of skin andnivolumab and
ipilimumab and cranial SRT (included only in the irradiated cohort) between 1
January 2016 and 31 December 2020. Exclusion criteria were defined by the
terms: vemurafenib or cobimetinib or dabrafenib or trametinib or craniectomy
for excision of brain tumor or stereotactic body radiation therapyor cranial
SRT (excluded only in the non-irradiated cohort).
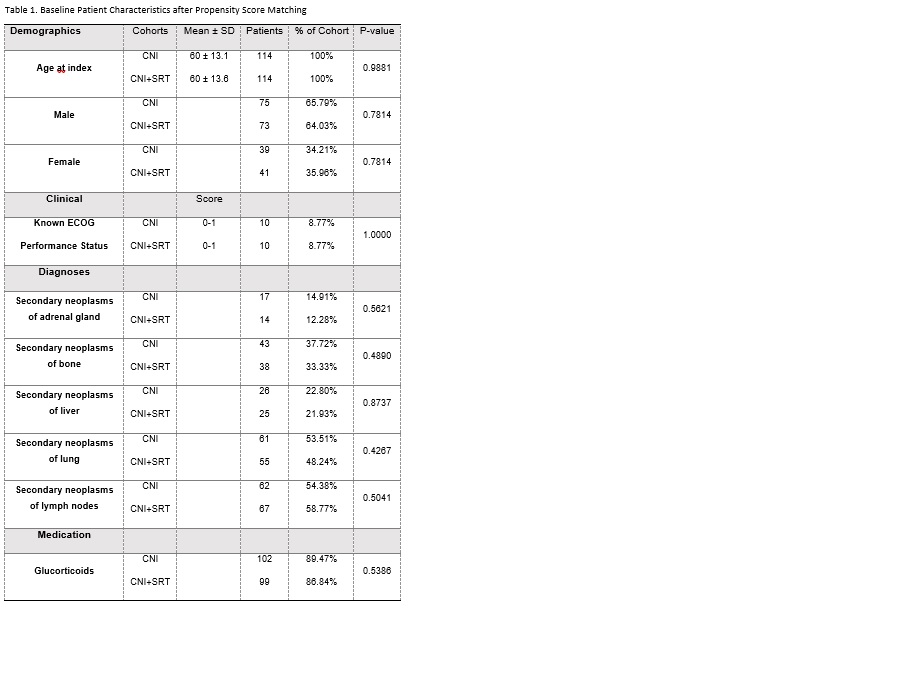
After building and retrieving the initial query for CNI and CNI+SRT cohorts, baseline characteristics were compared with chi‐squared
tests for categorical variables and independent‐sample
t tests for continuous variables. A propensity score matching was run to balance
cohorts with the following baseline characteristics: age, sex, known ECOG status, extracranial metastases (secondary malignant neoplasms of
adrenal gland, bone, liver, lung and lymph nodes) and use of glucocorticoids.
OS was defined from the date on which the patient met all selected criteria for
the cohort to date of death and estimated by Kaplan-Meier. Log-rank
test was applied to compare the survival curves. Hazard ratio (HR) with 95%
confidence intervals, together with the test for proportionality, was
calculated. Statistical significance was prespecified as P <.05
Results
The initial query retrieved 355 patients from
31 HCO in CNI cohort and 114 patients from 16 HCO in CNI+SRT cohort. After
propensity score matching, 114 patients were selected in each cohort. Baseline
characteristics are listed in Table 1. There
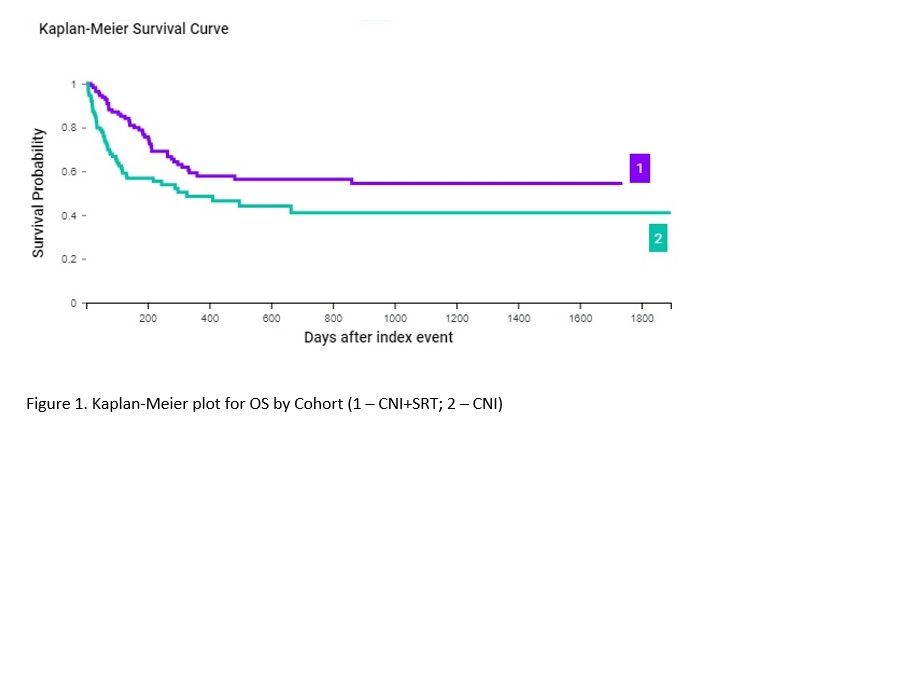
were 52 and 42 deaths in CNI and CNI+SRT cohort, respectively. The median OS
was 327 days in CNI and not reached in patients in CNI+SRT cohort, with a
probability of survival at end of time window of 54.4% and 40.9%, respectively
(log-rankP = .0057; Figure 1). Treatment with CNI+SRT was associated with a
significantly decreased mortality (HR, 0.57; 95% CI 0.377-0.853;
proportionality P = .0034).
Conclusion
This real-world, selective approach and propensity score matching analysis showed
that CNI+SRT led to an improvement in OS compared to CNI, corroborating prior
findings that local therapy with SRT or surgery improved OS in patients treated
with CNI for MBM, regardless
of the timepoint of local therapy.