Moderated hypofractionation in brain metastases and cerebral edema
Carmen Corral Fernandez,
Spain
PO-1146
Abstract
Moderated hypofractionation in brain metastases and cerebral edema
Authors: Corral Fernandez Carmen1, Vera Barragán Victoria2, González De Dueñas María2, Baños Pérez Beatriz2, Simón Silva Paula2, Ríos Kavadoy Yesika2, Quirós Rivero Juan2, Ropero Carmona Francisca2, Muñoz Garcia Julia Luisa2
1Universitary Hospital Badajoz, Radiation Oncoloy, Badajoz, Spain; 2Universitary Hospital Badajoz, Radiation Oncology, Badajoz, Spain
Show Affiliations
Hide Affiliations
Purpose or Objective
Brain metastases are the most frequent tumors in the central nervous system. Radiotherapy treatment (stereotactic radiotherapy) in a single fraction or in 2-10 fractions (hypofractionated radiotherapy) achieve good results in local control and moderate side effects. The most frequent side effects are edema worsening and radionecrosis (RN).
The pathophysiology of brain edema after radiotherapy remains unclear, although many factors could be linked as disruption of the blood-brain barrier, damage to microglia and astrocytes. In general, factors as the PTV volume, irradiation dose and the volume of brain receiving a specific dose are the main risk factors of RN.
To evaluate overall survival (OS), progression free survival (PFS) and relationship between the volume edema, volume PTVandtoxicity associated during the hypo fraction treatment and their evolution after treatment, a retrospective study was designed.
Material and Methods
Between 2019 and 2021 a total of 12 patients with 17 supratentorial metastases were reviewed. The 50% received radiotherapy to surgical bed, these were treated with total dose of 30 Gy in five fractions every other day and one of them 40Gy in 10 fractions due to the extense volume of treatment. Previous WBRT or radiosurgery were exclusion criteria.
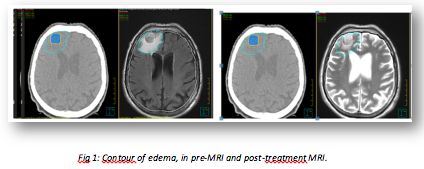
To study the relationship between brain volume irradiated and the edema post radiotherapy, the edema volume in both MRI was contoured. In the diagnosis MRI and in the first control (3 months since the end of the treatment). The image fusion was done in the planning system (Pinnacle) using the CT planning with the T2/FLAIR sequence in both MRI. (Fig. 1)
Results
The median follow-up for all patients was 9,4 months (2,1-24,2).
The most frequently histology was NSCLC (50%) followed by renal cancer (25%), mean age was 71 years (42-87). OS at 10 months of 79,5% and PFS of 52% at 10 months.
The median planning target volume (PTV) was 5,7cc (range 47,1-0,9 cc).
In the statistical analysis with IBM v.24, ANOVA analysis showed no statistical relationship between irradiated brain volume (V25 and V30) (p 0,8/0,3) or PTV volume (p 0,9) and time to relapse. A significative tendency between volume PTV and OS was observed. No severe toxicities were observed. The 50% of the patients presented in the first control a median reduction edema 19,6 cc (4,5-66cc) 66% of them could reduce the steroids dose after treatment. The major volume of PTV was linked with a minor edema reduction in the first image control.
Conclusion
Our study suggests no significative statistical relationship between brain volume irradiated or PTV and OS or PFS. 50% of patients reviewed experimented significative reduction of the edema volume in the MRI at 3 months after treatment. The 66% of the patients could reduce steroids dose. Hypofractionated scheme is a safe option of treatment for brain metastasis with impact over the reduction in steroids dose and brain edema after treatment.