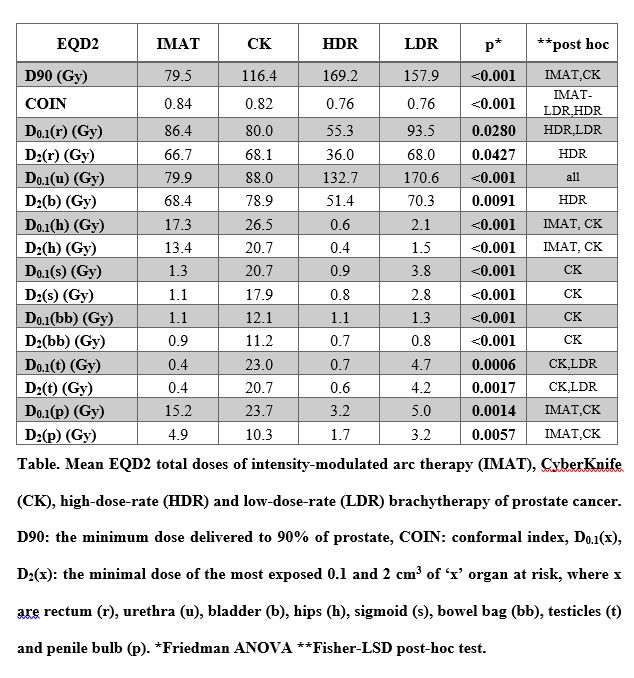
EQD2 total dose of the prostate was significantly lower with IMAT and
CK than with HDR and LDR BT, D90 was 79.5Gy, 116.4Gy, 169.2Gy and 157.9Gy
(p<0.001), respectively. However, teletherapy plans were more conformal than
BT, COIN was 0.84, 0.82, 0.76 and 0.76 (p<0.001), respectively. The D2
to rectum and bladder were lower with HDR BT than with IMAT, CK or LDR BT, it
was 66.7Gy, 68.1Gy, 36.0Gy and 68.0Gy (p=0.0427), and 68.4Gy, 78.9Gy, 51.4Gy
and 70.3Gy (p=0.0091) in IMAT, CK, HDR and LDR BT plans, while D0.1
to urethra was lower with both IMAT and CK than with BTs: 79.9Gy, 88.0Gy,
132.7Gy and 170.6Gy (p<0.001). D2 to hips was higher with IMAT
and CK, than with BTs: 13.4Gy, 20.7Gy, 0.4Gy and 1.5Gy (p<0.001), while D2
to sigmoid, bowel bag, testicles and penile bulb was higher with CK than with
the other techniques (Table).