Survival outcomes and patterns of failure from stage migration of FIGO staging in cervical cancer
Wiwatchai Sittiwong,
Thailand
PD-0911
Abstract
Survival outcomes and patterns of failure from stage migration of FIGO staging in cervical cancer
Authors: Wiwatchai Sittiwong1, Pittaya Dankulchai1, Nattapon Chareonsiriwat2, Soravit Manopetchkasem1, Tissana Prasartseree1
1Faculty of Medicine Siriraj Hospital, Radiology, Bangkok, Thailand; 2Faculty of Medicine Siriraj Hospital, Radiology, Bangkok , Thailand
Show Affiliations
Hide Affiliations
Purpose or Objective
The outcome of concurrent chemoradiation in combination with high dose rate image guided adaptive brachytherapy (HDR-IGABT) for cervical cancer was favorable. However, the transformation of staging from FIGO2009 to FIGO2018 which incorporated nodal status into stage IIIC contributed the migration of patients among stages. The objective of this study was to compare the treatment outcomes and patterns of failure stratified by different FIGO staging in HDR-IGABT era.
Material and Methods
363 patients treated with definitive external beam radiation (EBRT) with/without concurrent chemotherapy followed by HDR-IGABT were retrospectively reviewed. Staging classification was based on FIGO2009 and FIGO2018. Kaplan-Meier estimates at 5 years were analyzed for local control, nodal control, distant metastasis-free survival, and overall survival. Pattern of failure including local, nodal, and distant failure stratified by FIGO staging was reported.
Results
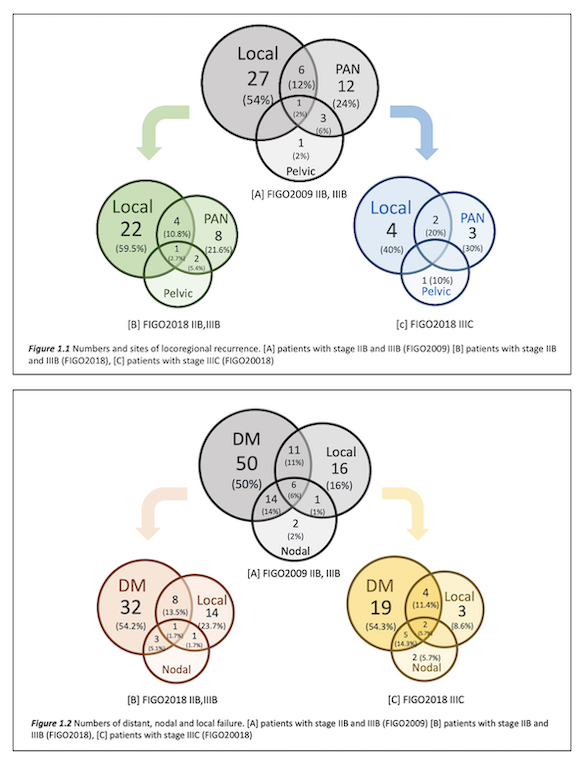
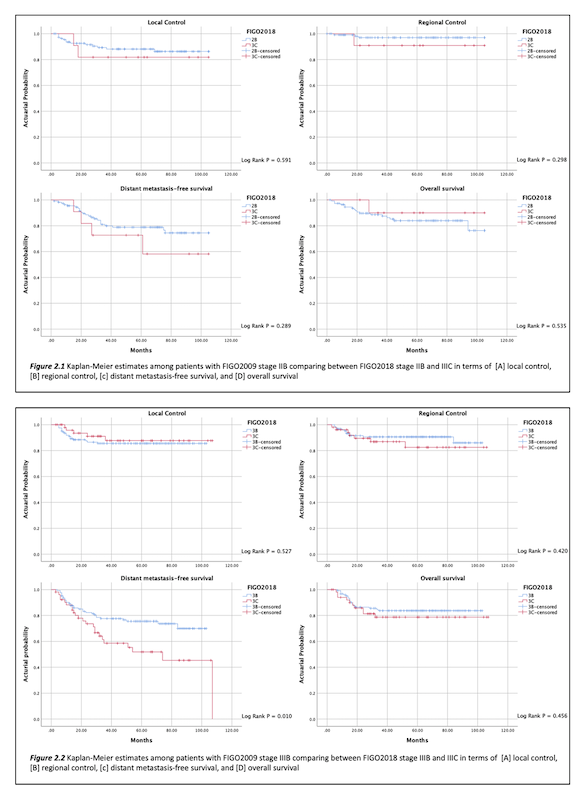
The median follow-up time was 52 months. According to FIGO 2009, patients were mainly diagnosed as stage IIB (123 patients, 33.9%) and IIIB (175 patients, 48.2%). Among patients with FIGO2009 stage IIB and IIIB, 11 of 123 patients (8.9%) of stage IIB and 52 of 175 patients (29.7%) of stage IIIB were staged as FIGO2018 IIIC. The rates of 5-year local control, nodal control, distant metastasis-free survival, and overall survival for the whole cohort were 86.6%, 92.1%, 73.5% and 84.2%, respectively. After incorporating stage migration into FIGO2009 stage IIB, there were no significant different between FIGO2018 stage IIB and IIIC in terms of local control, nodal control, distant metastasis-free survival, and overall survival. For FIGO2009 stage IIIB, there was a significant difference between FIGO2018 stage IIIB and IIIC for distant metastasis-free survival (p = 0.010) but similar local control, nodal control, and overall survival. For pattern of failure among patients FIGO2009 stage IIB and IIIB, the primary site was distant failure (81 patients, 81%). After separating FIGO2018 stage IIIC, distant failure was still predominant. The most common sites for distant metastasis were lung (30.7%), bone (12.8%), and intraabdominal lymph node (12.1%). For locoregional failure among patients with FIGO2009 stage IIB and IIIB, the primary site was local which was found in 34 patients (68%). After separating FIGO2018 stage IIIC, paraaortic node (PAN) and pelvic node recurrence were more prevailing than FIGO2018 stage IIB and IIIB.
Conclusion
Stage migration of cervical cancer from FIGO2009 to FIGO2018 contributed significantly different distant metastasis-free survival among patients with stage IIIB but not for stage IIB; whereas, local control, nodal control, and overall survival between FIGO2018 stage IIIC and IIB-IIIB were found no significant difference. The predominant site of failure was similar among different FIGO staging which was distant metastasis.