Bowel loop motion decreases during radiotherapy in gynaecological cancer patients using 3D cine-MRI
Janna Laan,
The Netherlands
PD-0905
Abstract
Bowel loop motion decreases during radiotherapy in gynaecological cancer patients using 3D cine-MRI
Authors: Janna Laan1, Lotte Ewals1, Zdenko van Kesteren1, Danique Barten1, Arjan Bel1, Henrike Westerveld1
1AmsterdamUMC, Radiation Oncology, Amsterdam, The Netherlands
Show Affiliations
Hide Affiliations
Purpose or Objective
Curative
radiotherapy for gynaecological cancer frequently results in bowel toxicity.
Bowel loop motion is not taken into account in radiotherapy planning, while it
may influence the actual dose received by individual bowel loops. Our primary
aim is to analyse bowel loop motion before External Beam Radiotherapy Treatment
(EBRT), after EBRT, and shortly before brachytherapy treatment with an
applicator in situ. Our secondary aim is to analyse the effect of different
patient and treatment characteristics that might influence bowel loop motion.
Material and Methods
A total of 20 women with gynaecological cancer treated
with definitive radiotherapy consisting of EBRT and brachytherapy were included.
During the treatment period three 10-minute 3D cine-MRI scans with an image
acquisition each 3.7s were obtained. The 1st before EBRT (MR1), the 2nd at the
end of EBRT (MR2), and the 3rd shortly after the brachytherapy applicator
insertion under general anaesthesia (MR3).
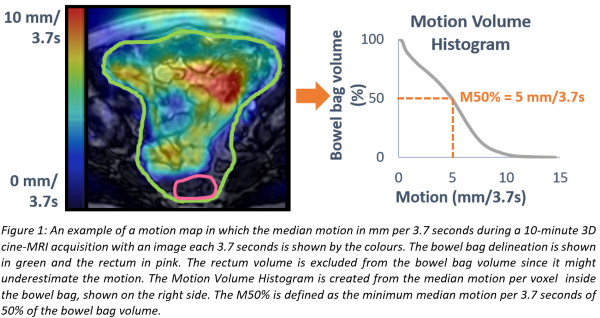
The
median bowel loop motion during the 10-minute scan was computed for all voxels
inside the bowel bag (Fig. 1). Motion Volume Histograms were created and from
these, the M50% (minimum motion per 3.7s of 50% of the bowel bag volume) was
computed as a measure for bowel loop motion (Fig. 1).
The difference in M50% before and
after EBRT (MR1 vs MR2), and the influence of fasting, general anaesthesia, and
the brachytherapy applicator (MR2 vs MR3) on M50% were analysed by the
Wilcoxon’s signed rank test. In addition, M50% before EBRT (MR1) was compared
between patients with and without previous abdominal surgery and between
patients with a BMI ≤25 vs >25 kg/m2 at
baseline. Furthermore, the influence of chemotherapy and BMI on the relative
difference in M50% before and after EBRT (MR1 and MR2) were analysed by Mann-Whitney
U tests.
Results
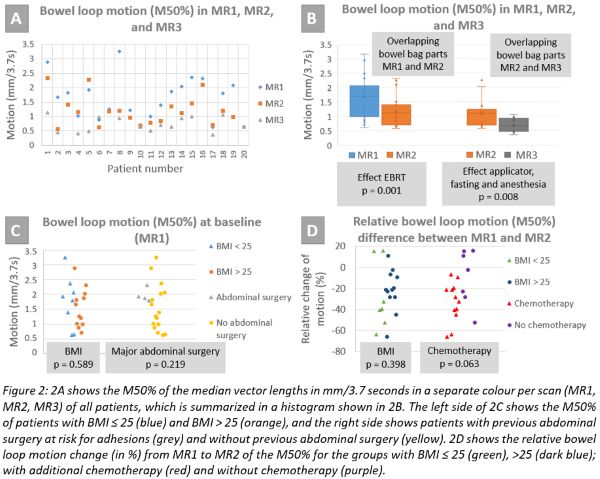
The median M50% (in mm per 3.7 seconds) of all
patients was 1.7 for MR1, 1.1 for MR2, and 0.7 for MR3, showing a significant
decrease in M50% between consecutive scans (p=0.001 for MR1 and MR2, and p=0.008
for MR2 and MR3)(Fig. 2AB). Neither previous abdominal surgery nor BMI were
associated with baseline M50% (Fig. 2C). In addition, BMI was not associated
with decreased M50% at the end of EBRT (Fig. 2D). There was, however, a
relative decrease in M50% of 31% at the end of EBRT in patients who received
chemotherapy, which was only 3% in patients who did not receive chemotherapy
(p=0.063)(Fig. 2D).
Conclusion
In our small cohort of patients treated for gynaecological
cancer, the median bowel loop motion decreased at the end of EBRT, and this was
even more pronounced at time of brachytherapy with an applicator in situ. In
addition, there is a trend towards a further decelerated bowel loop motion
after concurrent chemotherapy. This
study strengthens the need for further research aiming to control for bowel
loop motion in our future pelvic radiotherapy planning.