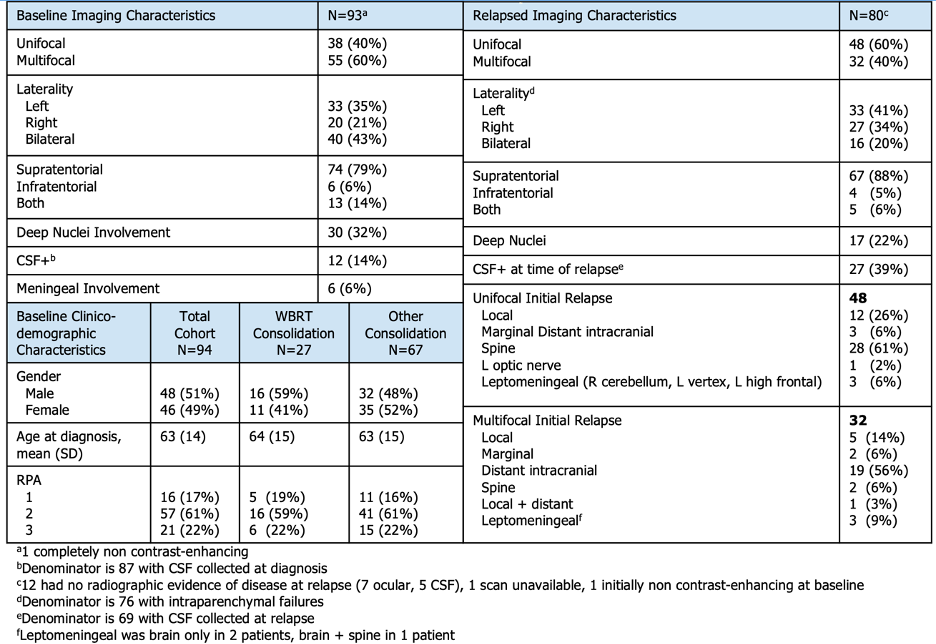
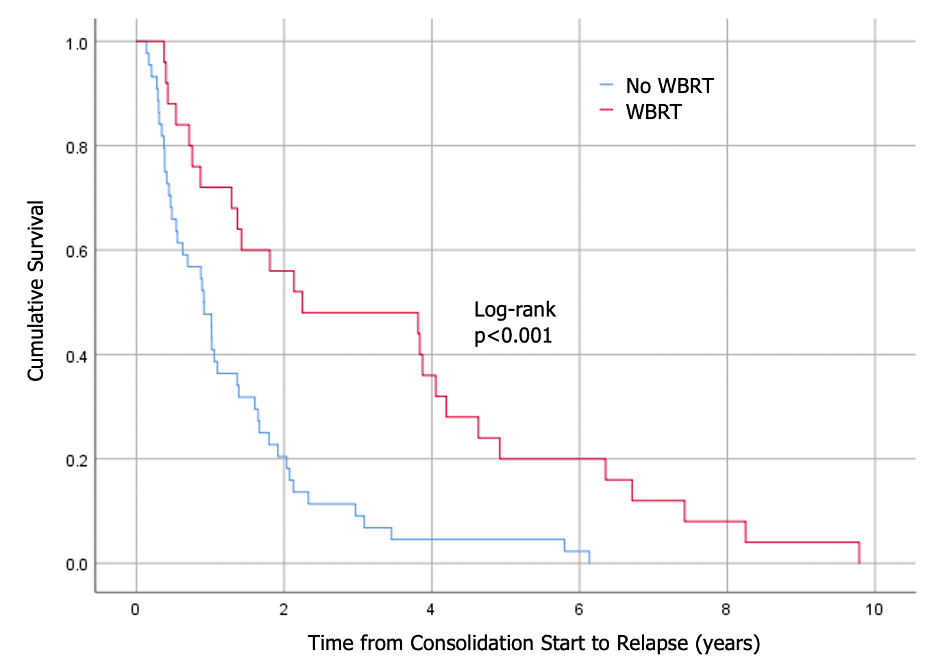
Of 259 patients treated with median follow-up of 3.7 years (range: 0.4-11.0), 94 (36%) relapsed at a median time of 1.3 years (range: 0.1-10.1) from induction initiation. Most received induction R-MVP (n=66, 70%) and most were consolidated (n=75, 80%), with cytarabine (n=42, 56%) or whole brain radiotherapy (WBRT, n=27, 29%). At baseline, most had multifocal (n=55, 60%) and supratentorial disease (n=74, 79%; Table). Fewer involved deep nuclei (n=30, 32%), meninges (n=6, 6%), or CSF (n=12 of 87 collected, 14%). At relapse, 80 (85%) had radiographic disease, 12 (13%) had cytologic evidence only (7 ocular on biopsy, 5 CSF involvement), and 2 (2%) scans were not evaluable. Of 80 radiographic relapses, most were supratentorial (61, 80%) and maintained laterality (17 of 33 [59%] ipsilateral left, 11 of 20 [55%] ipsilateral right). Intracranial failures (n=76) were mostly distant (n=54, 71%) with fewer relapsing both locally and unifocally (n=15, 20%). Patients with EOD pre-consolidation were more likely to have a local failure (OR 4.8 [95% CI 1.1-7.1], p=0.06). WBRT consolidation was associated with longer TTF (2.2 vs 0.9 years, p<0.001; Figure) and delivered mostly (n=23, 85%) with reduced dose (2340cGy/13fx). Median OS trended toward improved with WBRT consolidation (7.4 vs 4.2 years, p=0.056).