Proton therapy in mediastinal lymphoma patients in a nationwide cohort, using model-based selection
Bastiaan Ta,
The Netherlands
OC-0294
Abstract
Proton therapy in mediastinal lymphoma patients in a nationwide cohort, using model-based selection
Authors: Bastiaan Ta1, Stefan Hutschemaekers2,3, Anne Crijns4, Pietro Pisciotta4, Richard Canters1, Gloria Vilches Freixas1, Patricia Cambraia Lopes2, Anne Niezink4
1Maastro Clinic, GROW School for Oncology, Maastricht University Medical Center+, Department of Radiation Oncology (MAASTRO), Maastricht, The Netherlands; 2HollandPTC, Department of Radiation Oncology, Delft, The Netherlands; 3Haaglanden Medical Center, Department of Radiation Oncology, The Hague, The Netherlands; 4University Medical Center Groningen, Department of Radiation Oncology, Groningen, The Netherlands
Show Affiliations
Hide Affiliations
Purpose or Objective
Since 2019 mediastinal lymphoma (ML) patients in
the Netherlands are treated with intensity modulated proton therapy (IMPT)
using model-based selection (MBS). MBS was performed according to the Dutch
national indication protocol for proton therapy. For ML this is based on the difference
in normal tissue complication probability (ΔNTCP) for lifetime acute coronary
events (ACE). The objective of this study was to evaluate dose advantages of
both qualifying and non-qualifying patients. We evaluated the feasibility of MBS
and the limitations of this approach by evaluating doses to other organs at
risk (OARs) relevant for induction of secondary tumours of which currently no NTCP
models are available.
Material and Methods
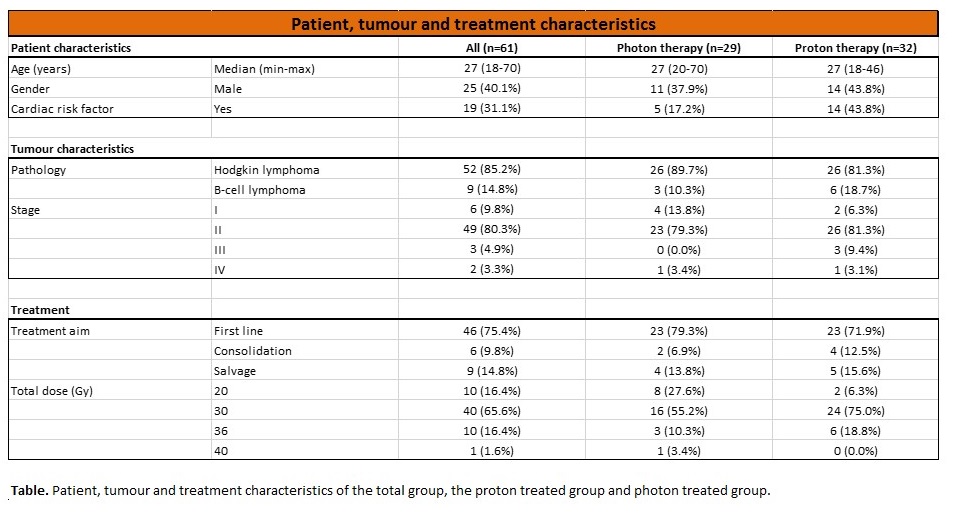
All 61 ML patients referred for plan comparisons (VMAT vs IMPT) to one of the three Dutch proton centres were included in this study. In each patient, the estimated clinical benefit in terms of ΔNTCP is derived from both treatment plans using the ACE NTCP model which includes mean heart dose (MHD), age, gender and risk factors for ACE as predictors. The ΔNTCP threshold for MBS is a 2% reduction for ACE. The differences in MHD, lungs (MLD) and oesophagus (MED) were evaluated. Finally, the reduction in mean breast dose (MBD) was investigated in female patients.
Robust IMPT plans were created using two to eleven beams depending on the target volume and a 3D robustly optimised planning technique was used. Radiotherapy consisted of 20-36 Gy in 2 Gy fractions and chemotherapy consisted of 3-4 cycles of A(B)VD or escBEACOPP for Hodgkin lymphoma or 6x R-CHOP for B-cell lymphoma.
Results
Thirty-two out of 61 patients (52%)
referred for plan comparisons met the predefined ΔNTCP threshold and were
eligible for IMPT (Table). In patients
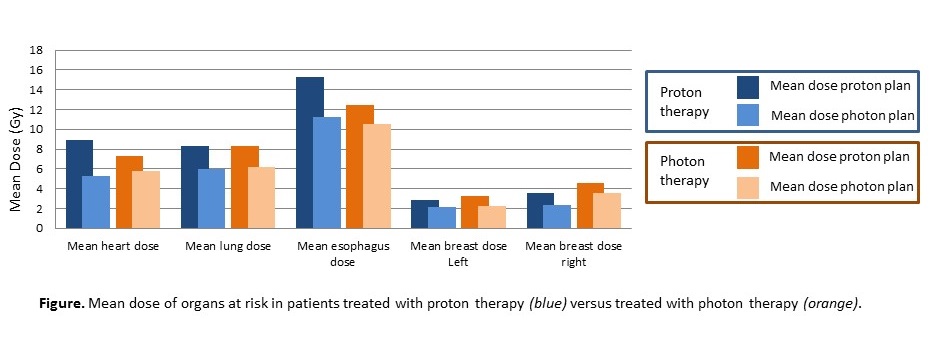
qualifying for IMPT, IMPT resulted in a significantly lower MHD (8.9 Gy vs. 5.3
Gy; p<0.01), MLD (8.3 Gy vs. 6.0
Gy; p<0.01), MED (15.3 Gy vs. 11.2
Gy; p<0.01), MBD-right (2.9 Gy vs.
2.1 Gy; p=0.001) and MBD-left (3.6 Gy
vs. 2.3 Gy; p=0.004). Using the NTCP
model for ACE, the mean NTCP for VMAT was 12.1% (range 2.1 – 30.4%) compared to
8.6% (range 0.1– 27.4%) for IMPT, an average ΔNTCP with IMPT for ACE of 3.4% (range
2.0 – 9.8; p<0.01). In patients
that did not qualify for IMPT, the dose to all OARs was also significantly
reduced; MHD (7.3 Gy vs. 5.8 Gy; p<0.01), MLD (8.3 Gy vs. 6.2 Gy; p<0.01), MED (12.5 Gy vs. 10.5 Gy; p=0.004), MBD-right (3.3 Gy vs. 2.2 Gy; p=0.012) and MBD-left (4.6 Gy vs. 3.6
Gy; p=0.014) (Figure).
Conclusion
Model-based selection of ML patients for proton therapy
is feasible. IMPT resulted in a significant MHD reduction and a subsequent 3.4% reduction in estimated lifetime risk of ACE. However,
patients not qualifying for proton therapy could benefit from proton therapy as
we found a significant reduction in dose to several OARs relevant for the
induction of cardiac complications and secondary tumour induction. Tools are
needed to further optimise patient selection.