Do clinical pathways facilitate contouring guideline use among radiation oncologists?
PO-1038
Abstract
Do clinical pathways facilitate contouring guideline use among radiation oncologists?
Authors: Diana Lin1, Sushil Beriwal2, James Murphy3, Erin Gillespie1
1Memorial Sloan Kettering Cancer Center, Department of Radiation Oncology, New York, USA; 2Allegheny Health Network, Department of Radiation Oncology, Allegheny, USA; 3University of California San Diego, Department of Radiation Medicine and Applied Sciences, La Jolla, USA
Show Affiliations
Hide Affiliations
Purpose or Objective
Contouring guidelines have been shown to reduce contour variability and improve predicted clinical outcomes, but are often underused. Clinical pathways are evidence-based decision support tools accessible from within electronic health records that integrate patient- and disease-specific information to generate treatment recommendations. While clinical pathways are used by 42% of medical oncologists in the United States, they are only used by approximately 7% of radiation oncologists. We hypothesized that clinical pathways would facilitate contouring guideline usage among practicing radiation oncologists.
Material and Methods
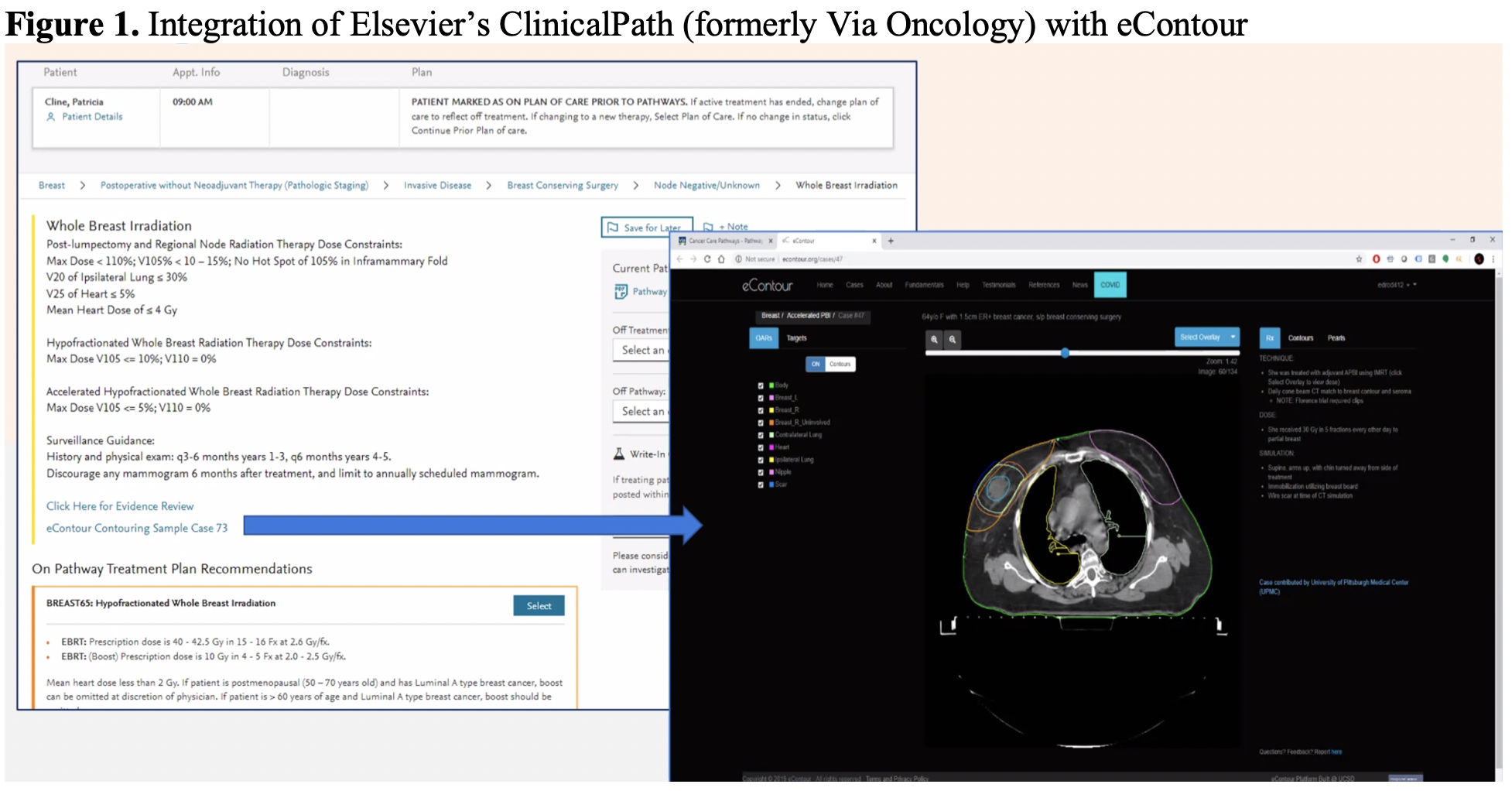
This is a prospective observational case-control study that assessed contouring guideline use among radiation oncologists in the United States registered on eContour.org. In 2019, clinical pathway vendor ClinicalPath (formerly Via Oncology) began providing direct links within disease-specific pathways to eContour, an open-access online platform displaying image-based contouring guidelines (Figure 1). The primary exposure was clinical pathway use (ClinicalPath) and primary outcome was eContour case page views. Subjects in the intervention group were matched 1:2 to those in the control group based on profession (practicing physician), country (United States), and years of experience (defined by medical school graduation year). The matched control group included a randomly selected sample of 50 out of the 3,085 practicing radiation oncologists located in the US that are registered on eContour. Mixpanel software was used to collect eContour usage statistics. Statistical testing included Wilcoxon rank sum test for the comparison of case views per month between the two study cohorts and Fisher’s exact test for the comparison of the distribution of case views between these two groups.
Results
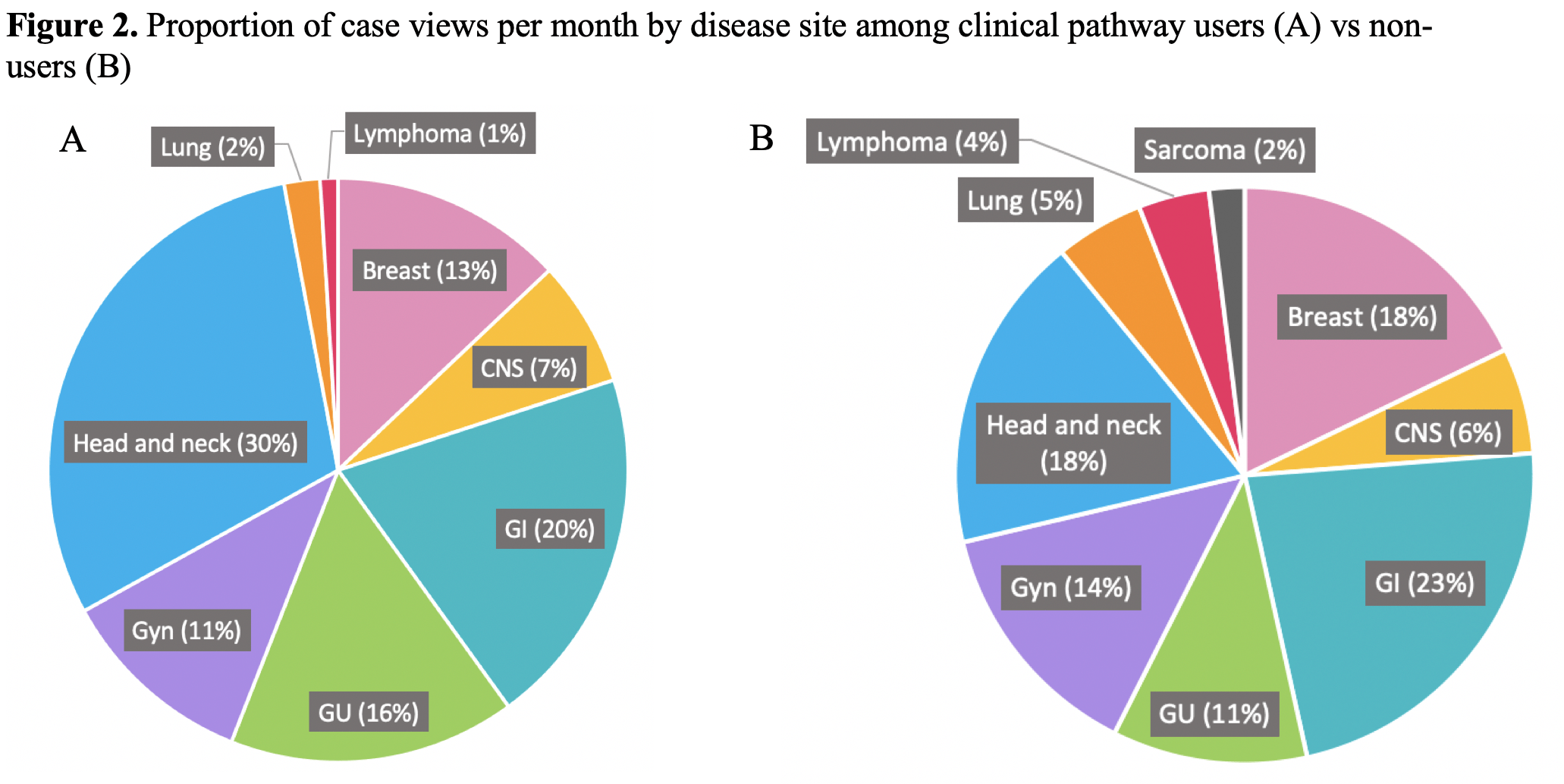
Forty-four eContour case links were inserted into clinical pathways from May 2019 to June 2020. Among 242 physician users of the clinical pathways, 32 (13%) were registered eContour users, of which 25 are practicing physicians (the intervention cohort); 7 residents were excluded from the analysis. Since March 2020, there have been 76 eContour link clicks through the clinical pathway. The median years of experience among practicing physicians was 27 years (IQR 14, 33) in the intervention cohort (n=25) vs 27 years (IQR 12, 35) in the control group (n=50). Since April 2021, there was no difference in case views per month among physicians in the intervention group compared to those in the control group (9+/-8 vs 10 +/-6, respectively, p=0.44). Head-and-neck and gastrointestinal were the most commonly-viewed cases and there was no difference in the distribution of case views between the intervention and control groups (p=0.26, Figure 2).
Conclusion
Hyperlinks within clinical pathways do not appear to be an effective strategy to facilitate contouring guideline use. Strategies that better coincide with the time of active contouring should be investigated.