Artificial Intelligence based planning of HDR prostate brachytherapy: first clinical experience.
PD-0821
Abstract
Artificial Intelligence based planning of HDR prostate brachytherapy: first clinical experience.
Authors: Danique Barten1, A. Bouter2, N. van Wieringen1, B.R. Pieters1, K.A. Hinnen1, G.H. Westerveld1, S.C. Maree2, M.C. van der Meer1, T. Alderliesten3, P.A.N. Bosman2, Y. Niatsetski4, A. Bel1
1Amsterdam UMC, University of Amsterdam, Radiation Oncology, Amsterdam, The Netherlands; 2Centrum Wiskunde & Informatica, Life Sciences and Health Group, Amsterdam, The Netherlands; 3LUMC, Radiation Oncology, Leiden, The Netherlands; 4Elekta, -, Veenendaal, The Netherlands
Show Affiliations
Hide Affiliations
Purpose or Objective
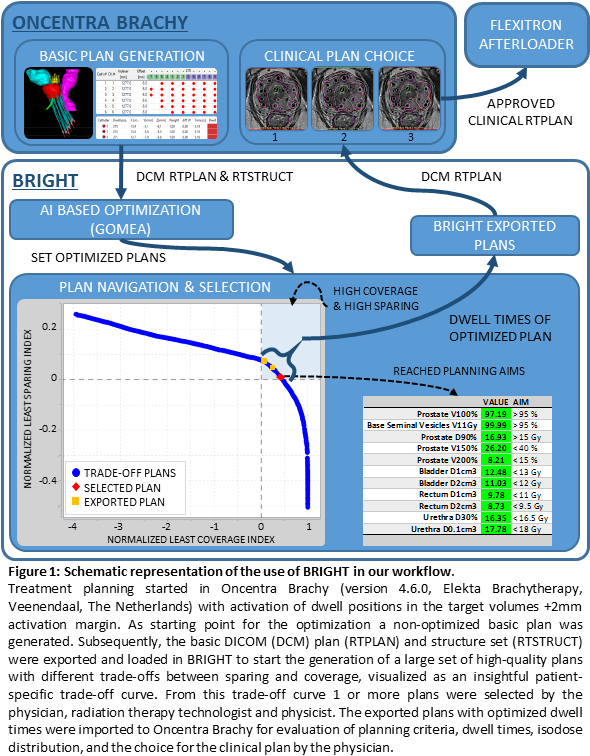
In
March 2020, we clinically introduced ‘BRachytherapy via artificially
Intelligent GOMEA-Heuristic based Treatment planning’ (BRIGHT) for
prostate cancer patients. The intention behind BRIGHT is to overcome a time-consuming
and unintuitive planning process, by automatically creating a set of high-quality
treatment plans from which the physician can choose the preferred plan per
patient. The purpose of this study is to evaluate the first clinical experiences
with Artificial Intelligence (AI) based planning for HDR prostate plans.
Material and Methods
Between
March 2020 and January 2021, 7 prostate cancer patients were treated in our centre
with single-dose HDR brachytherapy (BT) with a dose of 15 Gy. After
implantation, MRI acquisition, catheter reconstruction, and delineation of the
target volumes and organs at risk, BRIGHT was used for treatment planning (TP)
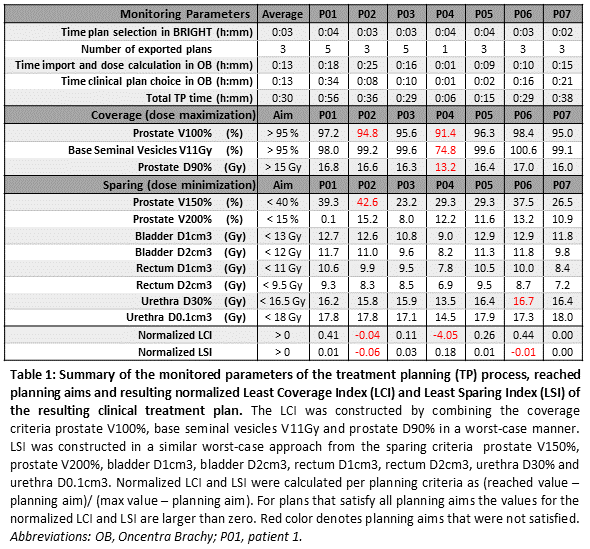
(Fig. 1). BRIGHT consists of a bi-objective planning model, in which the TP aims
(Table 1) are grouped into one coverage objective and one sparing objective,
referred to as the Least Coverage Index (LCI) and Least Sparing Index (LSI).
These were constructed in a worst-case manner: For example, an
LCI = 2.0% means that all targets are covered at least 2.0% more than
their planning-aim. BRIGHT’s graphical user interface allows navigation over the coverage-sparing trade-off curve and allows to make a selection for further
dose-calculation and clinical plan determination in Oncentra Brachy. For each
patient the plan selecting aspects and process times were monitored (Table 1).
Results
For all patients, multiple
plans that satisfied all planning aims could be selected in BRIGHT. Table 1
summarizes the results of the monitored parameters, reached planning aims, and LCI/LSI
of the resulting clinical treatment plan for each patient. Time was spent on manual
optimization of the BRIGHT plan before clinical plan approval to reduce large
dwell times that caused undesired large high-dose sub-volumes in the target. Parameters
of influence on the clinical plan choice were: Patient-specific clinical
information, knowledge of the trade-off curve, dwell time pattern, and isodose
distribution. As example: Based on these parameters the focus in patient 4 was on
sparing of the urethra due to urinary complaints and the decision was made to underdose
the target. In patient 2 a catheter was found incorrectly reconstructed, after
correction the plan was not re-optimized in BRIGHT due to time pressure,
resulting in a higher prostate V100%.
Conclusion
The
users appreciated the intuitive process of navigating the trade-off curve to
select the best solution for a patient. To improve time efficiency user
training is on-going and additional planning criteria need to be implemented to
improve plan quality, e.g. dose homogeneity and normal tissue dose constraints.
After one year of clinical experience, we can conclude that AI based TP for HDR
prostate BT is successfully implemented in our clinic and is a promising tool for
further applications in BT.