Quality of life, toxicity, and PSA control after 50 Gy SBRT to the dominant intraprostatic nodule
PD-0764
Abstract
Quality of life, toxicity, and PSA control after 50 Gy SBRT to the dominant intraprostatic nodule
Authors: Minna Cloitre1, Massimo Valerio2, Beat Roth2, Dominik Berthold 3, Thomas Tawadros2, Jean-Yves Meuwly4, Leonie Heym1, Frederic Duclos 5, Stephanie Viguet-Carrin 6, Veronique Vallet 1, Jean Bourhis5, Fernanda Herrera1
1Lausanne University Hospital , Radiation Oncology, Lausanne, Switzerland; 2Lausanne University Hospital , Urology, Lausanne, Switzerland; 3Lausanne University Hospital , Oncology, Lausanne, Switzerland; 4Lausanne University Hospital , Radiology and Interventional Radiology, Lausanne , Switzerland; 5Lausanne University Hospital , Radiation Oncology, Lausanne , Switzerland; 6Lausanne University Hospital , Center for Experimental Therapeutics, Lausanne , Switzerland
Show Affiliations
Hide Affiliations
Purpose or Objective
Stereotactic body radiation therapy (SBRT) yields excellent disease control for low- and intermediate-risk prostate cancer (PCa). However, the current evidence of biochemical disease-free survival (bDFS) and toxicity in high-risk (HR) disease is scarce. Localized prostate cancer is multifocal; however, the dominant intra-prostatic nodule (DIN) is responsible for disease recurrence after radiation therapy. We report 4-year update on treatment toxicity, quality of life (QOL), and PSA control from 28 patients (60% with HR-PCa) treated with up to 50 Gy SBRT to the DIN in the context of a phase I/II study.
Material and Methods
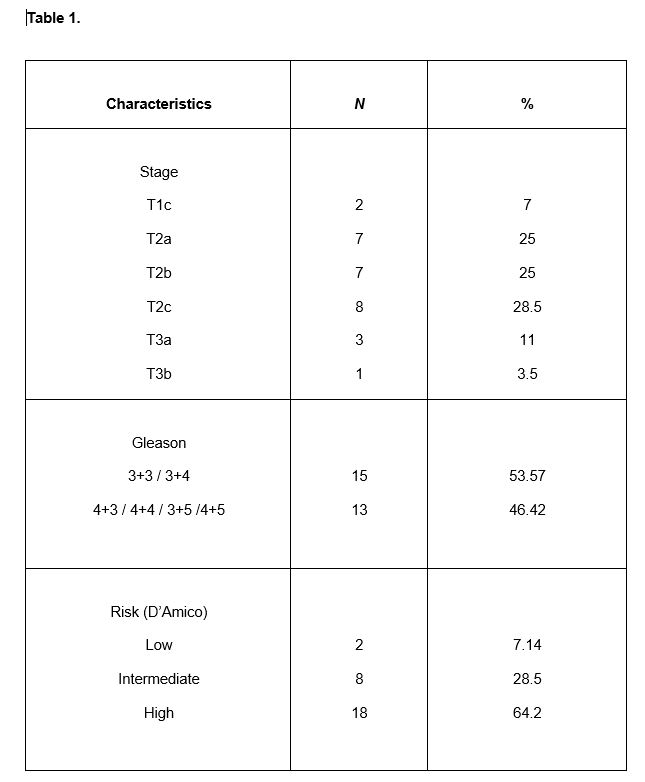
28 patients with localized PCa underwent an absorbable peri-rectal balloon spacer (BioProtect Ltd., Tzur Yigal, Israel) insertion under general anesthesia and were subsequently treated with SBRT doses of 36.25 Gy in 5 fractions to the whole prostate while simultaneously escalating doses to the magnetic resonance image visible DIN (45 Gy, 47.5 Gy, and 50 Gy in five fractions). The treatment was delivered with CyberKnife (Accuray Inc, Sunnyvale, CA, USA). Phase I part was designed to determine the recommended phase II dose (RP2D) in a 3 + 3 cohort-based dose escalation design. Primary endpoint: Dose-limiting toxicities (DLT) defined as grade 3 or worse gastrointestinal (GI) and/or genitourinary (GU) toxicity by Common Terminology Criteria of Adverse Events (version 4) up to 90 days after the first radiation fraction. Secondary endpoints: biochemical control, QOL, and dosimetry outcome. Patient’s characteristics are represented in Table 1.
Results
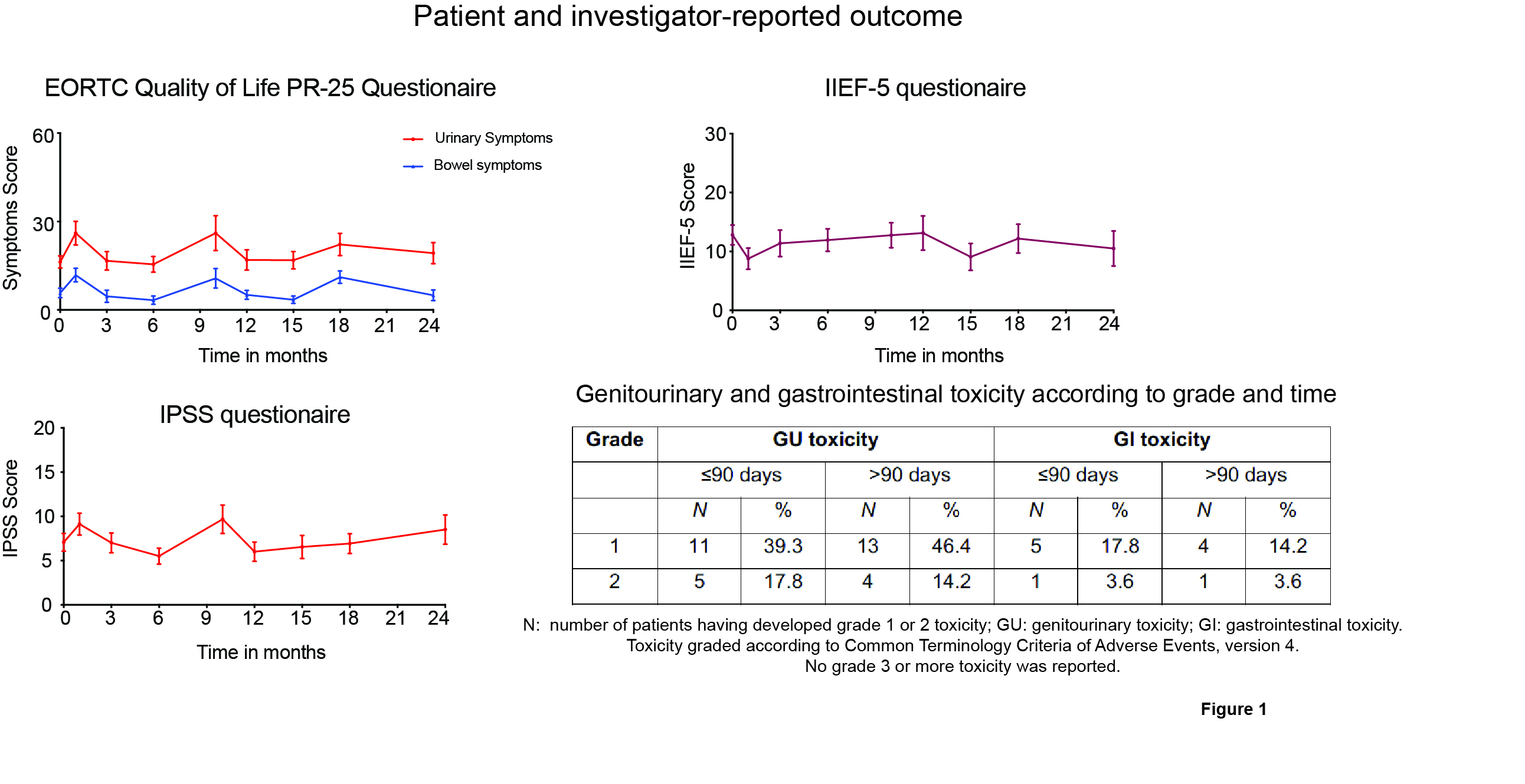
No spacer procedure-related AEs were reported. 9 patients were treated in the phase I part. No DLT was observed at either level and therefore the maximum tolerated dose was not reached. Further characterization of tolerability and efficacy were conducted in the subsequent 19 patients irradiated at the highest dose level (50 Gy, RP2D) in the phase II cohort. At a median follow-up of 52 months, biochemical control is 83%. Grade 1 and 2 acute GU and GI toxicity was 39.3% and 17.8%, and 17.8% and 3.6%, respectively. G1 and 2 late GU and GI toxicity was 46.4% and 14.2%, and 14.2% and 3.6%, respectively. No grade 3 or higher toxicity was reported. Quality of life data is presented in Figure 1. Median maximum dose (0.1 cm3) were: to rectum <33 Gy (range 26-41 Gy), to bladder <38 Gy (range 37.5-41 Gy), and to the urethra<38 Gy (range 35-41 Gy), which fully complied with protocol.
Conclusion
Irradiation of the whole prostate with 36.25 Gy in 5 fractions and dose escalation to 50 Gy to the DIN, when combined with peri-rectal balloon spacer, was tolerable and determined as RP2D. This treatment has promising anti-tumor activity in patients with HR-PCa. QOL analysis showed minimal negative impact in GU, GI, and sexual domains. No complications were observed due the insertion of a peri-rectal balloon spacer. Compliance with protocol dose prescriptions was 100%.