Dose escalation is feasible in short course radiotherapy of rectal cancer – a planning study
Lynsey Devlin,
United Kingdom
OC-0648
Abstract
Dose escalation is feasible in short course radiotherapy of rectal cancer – a planning study
Authors: Lynsey Devlin1, Bianca Hunter2, Hiwot Chemu1, Philip McLoone3, Ronan Valentine2, Paul Cornelious2, Aileen Duffton1, Sean O'Cathail4
1Beatson West of Scotland Cancer Centre, Radiotherapy, Glasgow, United Kingdom; 2Beatson West of Scotland Cancer Centre, Department of Radiotherapy Physics, Glasgow, United Kingdom; 3Institute of Health & Wellbeing, University of Glasgow, Glasgow, United Kingdom; 4Institute of Cancer Sciences,, University of Glasgow, Glasgow, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
Short course radiotherapy (SCRT) with 5x5Gy followed by chemotherapy is a new standard of care for locally advanced rectal cancer 1.
Given the low biological dose of this prescription; the existence of a dose response; and the moderate α/β ratio (~5) of rectal cancer, we hypothesise that hypofractionated dose escalation would have significant radiobiological advantages. We assessed the in-silico feasibility of dose escalation to the primary tumour up to 35Gy using a simultaneous integrated boost (SIB), conserving OAR constraints.
Material and Methods
Patients immobilised in supine position had a planning CT (2-2.5mm, L2/3 to mid-femur) with bowel and bladder preparation and intravenous contrast.
GTV was macroscopic tumour including rectal lumen. CTVA was GTV + 10mm margin. CTVB was elective nodes (mesorectal, presacral, obturator and internal iliac). PTV_Low was created from CTVF (CTVA + CTVB) + 7mm margin. PTV_High (SIB) was created from GTV + 5mm margin.
OAR (bladder, small bowel loops, bowel cavity) were delineated as per RTOG guideline definitions. All structures were delineated by Clinical Oncologists and peer reviewed. Each patient had 4 plans produced at increasing dose levels to the SIB volume (PTV_High) 27.5Gy, 30Gy, 32.5Gy and 35Gy. The dose prescribed to PTV_Low was 25Gy in 5 fractions.
Plans were inverse planned with energy of 6MV on a Varian Truebeam (2.7) in Eclipse v15.5 using PO v15.5 for inverse planning, Acuros v15.5 for final calculation and DVH estimation algorithm v15.5. Feasibility was defined as 90% of plans achieving the planning objectives at 32.5Gy dose level (EQD2 53.2Gy).
Results
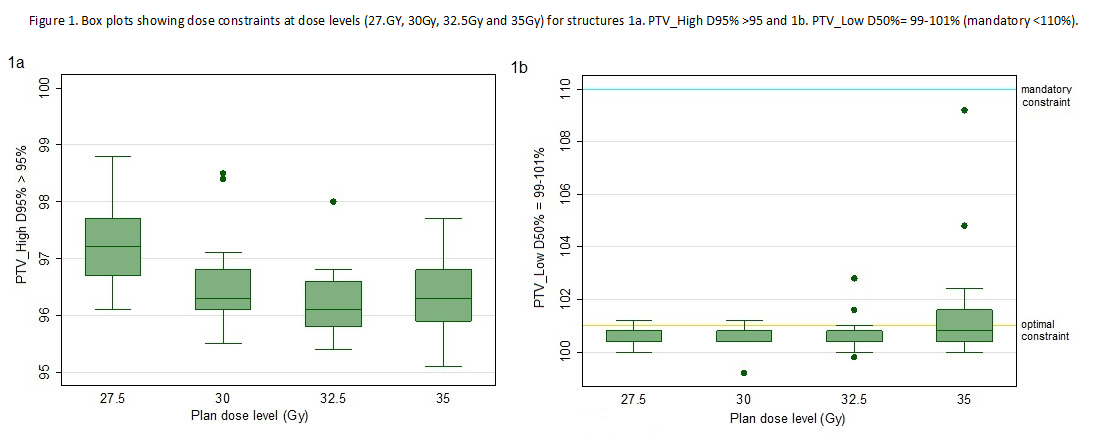
19 rectal cancer SCRT patients were anonymised and included in the study. Patient median age was 70 (IQR 60.75-77), F (n=4), M (n=15). Rectum level was low (n=10), mid (n=4) and upper (n= 5). A total of 95 treatment plans were analysed. The mean volume was 130cm3 (SD 81.5) and 769.6cm3 (SD 241.1) for PTV_High and PTV_Low respectively. Table 1.shows all 95 plans complied with the planning constraints at the dose metrics for each structure at the 25 Gy plan and each dose level (27.5Gy, 30Gy, 32.5Gy and 35Gy). Figure 1a. shows all patients achieved the planning constraint for PTV_High D95% > 95% at each dose level. Figure 1b. shows for PTV_Low D50% = 99-101% the majority of plans achieved the optimal constraint up to the 32.5.Gy level and at 35Gy dose level all plans were within mandatory constraints.

Conclusion
Hypofractionated dose escalation to the primary tumour up to 35Gy is feasible in SCRT for rectal cancer. All plans met our a priori definition of feasibility at 32.5Gy (EQD2 53.2Gy). Above this at the 35Gy level, dose to PTV_Low exceeded the optimal constraints, but achieved mandatory. Future analysis will explore this effect.
1.Bahadoer et. al. SCRT followed by chemotherapy before total mesorectal excision versus preoperative chemoradiotherapy, TME, and optional adjuvant chemotherapy in locally advanced rectal cancer (RAPIDO): Lanc Oncol.2021;22(1):29-42.