Radiographer-led online image guided adaptive radiotherapy: A qualitative investigation
Elizabeth Joyce,
United Kingdom
OC-0615
Abstract
Radiographer-led online image guided adaptive radiotherapy: A qualitative investigation
Authors: Elizabeth Joyce1, Helen A McNair1,2, Geraldine O'Gara3, Marcus Jackson4, Bianca Peet5, Robert A Huddart2, Theresa Wiseman3
1Royal Marsden Hospital, Radiotherapy, London, United Kingdom; 2Institute of Cancer Research, Radiotherapy and Imaging, London, United Kingdom; 3Royal Marsden Hospital, Health Research, London, United Kingdom; 4St George's University of London, Radiography, London, United Kingdom; 5Royal Marsden Hospital, Clinical Trials, London, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
Online MRI guided adaptive radiotherapy (MRIgRT)
is resource intensive. To maintain and increase uptake, traditional roles and
responsibilities may need refining. This novel study aims to provide an
in-depth understanding and subsequent impact of the roles required to deliver
MRIgRT.
Material and Methods
A purposive sampling approach was used to invite
radiographers, clinicians and physicists from centres with varied experience of
MRIgRT. Respondents from six centres participated in Focus Group Interviews
(FGIs). FGIs were chosen to allow researchers to obtain several perspectives and
reach consensus and were conducted with two facilitators using a semi-structure
interview guide. Four researchers independently familiarised themselves and
coded the data using framework analysis. A consensus thematic framework of
codes and categories was agreed and systematically applied.
Results
Thirty participants took part (Radiographers: n=18,
Physicists: n=9 and Clinicians: n=3). Three key themes were identified:
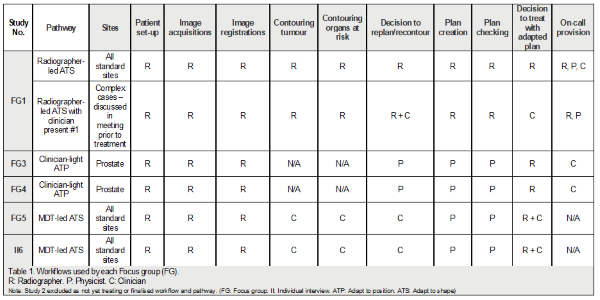
‘Current MRIgRT’, ‘Training’ and ‘Future Practice’. Current MRIgRT identified a
variation in radiographers’ roles and responsibilities with pathways ranging
from radiographer-led, clinician-light-led and MDT-led as seen in Table 1.
The consensus was to move towards
radiographer-led with the need to have a robust on-call service heavily
emphasised. The importance of continuity and relevant staff only to be present
in designated areas when treatment is undertaken was highlighted. The breadth
of knowledge required by radiographers including MRI, contouring, planning and
dosimetry, and treatment experience was highlighted. Debate was presented over
timing and length of training required. There was dispute over whether training
should be delivered pre-MRIgRT exposure or on-the-job, but it was agreed that a
blended approach was preferred by all. Future Practice identified the
need to have radiographers solely deliver MRIgRT, to reduce staff present which
was a main driver by all interviewed. Radiographers reported their enthusiasm
for this role and physicists envisioned this happening. Clinicians and
Physicists disclosed they had sufficient confidence in radiographers to do
this. Time and resources to train radiographers were the main barriers with an
emphasis placed on the difficulty of arranging consistent training and lack of
MDT availability to deliver it.
Conclusion
Radiographer-led MRIgRT is an exciting
development because of the potential radiographer role development. Roles must
be created with sufficient support and robust governance to enable evaluation
of effectiveness, impact, ongoing sustainability and responsiveness. A national
training framework created collaboratively with all stakeholders and
professions involved would ensure consistency in skills and knowledge.