Tumour Repopulation Varies Between Sequential vs. Concurrent Chemoradiation in Lung Cancer
OC-0527
Abstract
Tumour Repopulation Varies Between Sequential vs. Concurrent Chemoradiation in Lung Cancer
Authors: Huei-Tyng Huang1, Michael G. Nix2, John D. Fenwick3,4, Maria A. Hawkins1
1University College London, Faculty of Engineering, Department of Medical Physics and Biomedical Engineering, London, United Kingdom; 2Leeds Teaching Hospitals NHS Trust, Leeds Cancer Centre, Department of Medical Physics and Engineering, Leeds, United Kingdom; 3University of Liverpool, Institute of Translational Medicine, Department of Molecular and Clinical Cancer Medicine, Liverpool, United Kingdom; 4Clatterbridge Cancer Centre, Department of Physics, Wirral, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
Chemoradiotherapy is the standard
of care for treating inoperable locally-advanced non-small cell lung cancer
(LA-NSCLC). We aim to investigate new models of survival following
treatment for LA-NSCLC incorporating the effects of chemotherapy.
Material and Methods
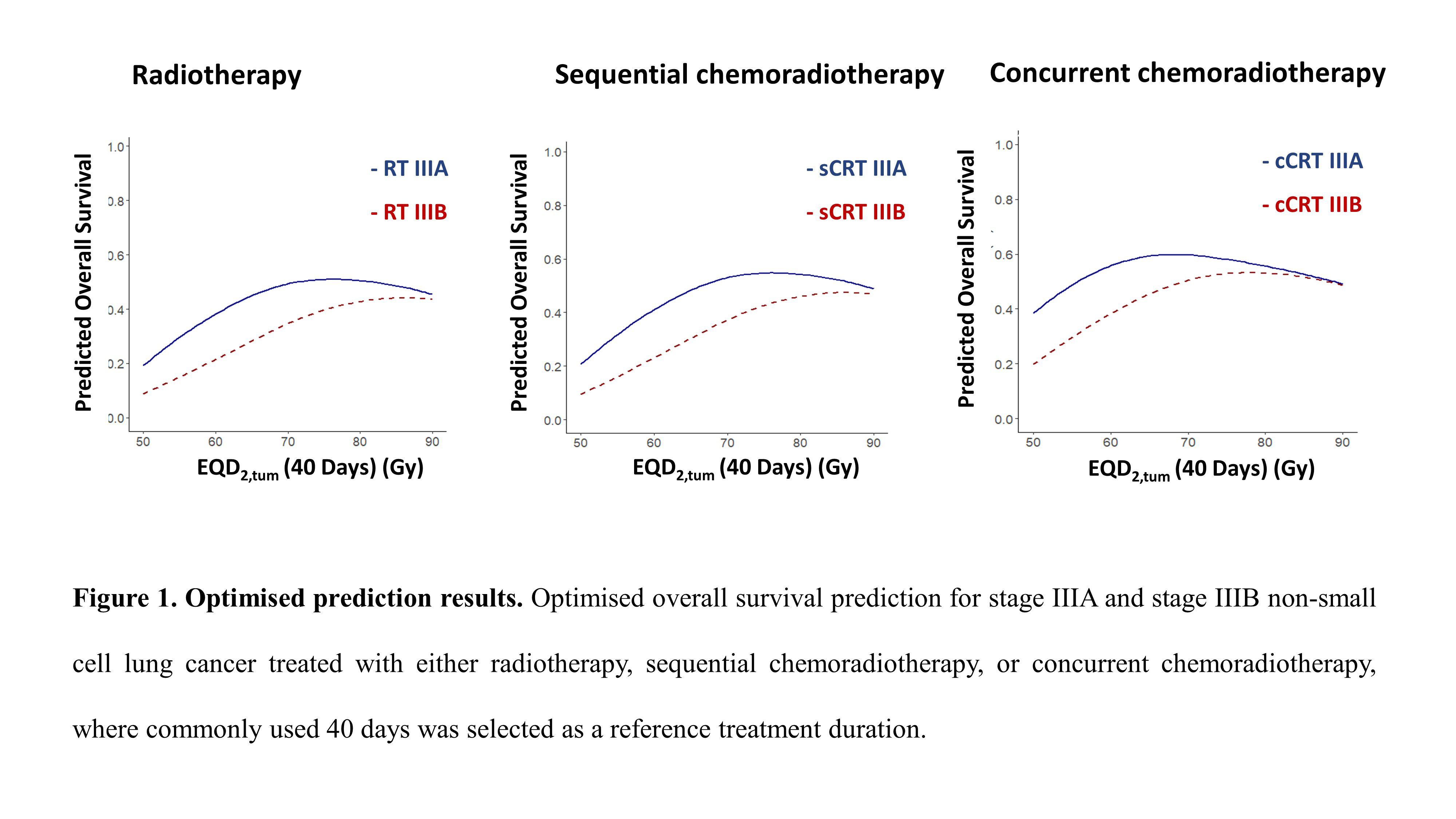
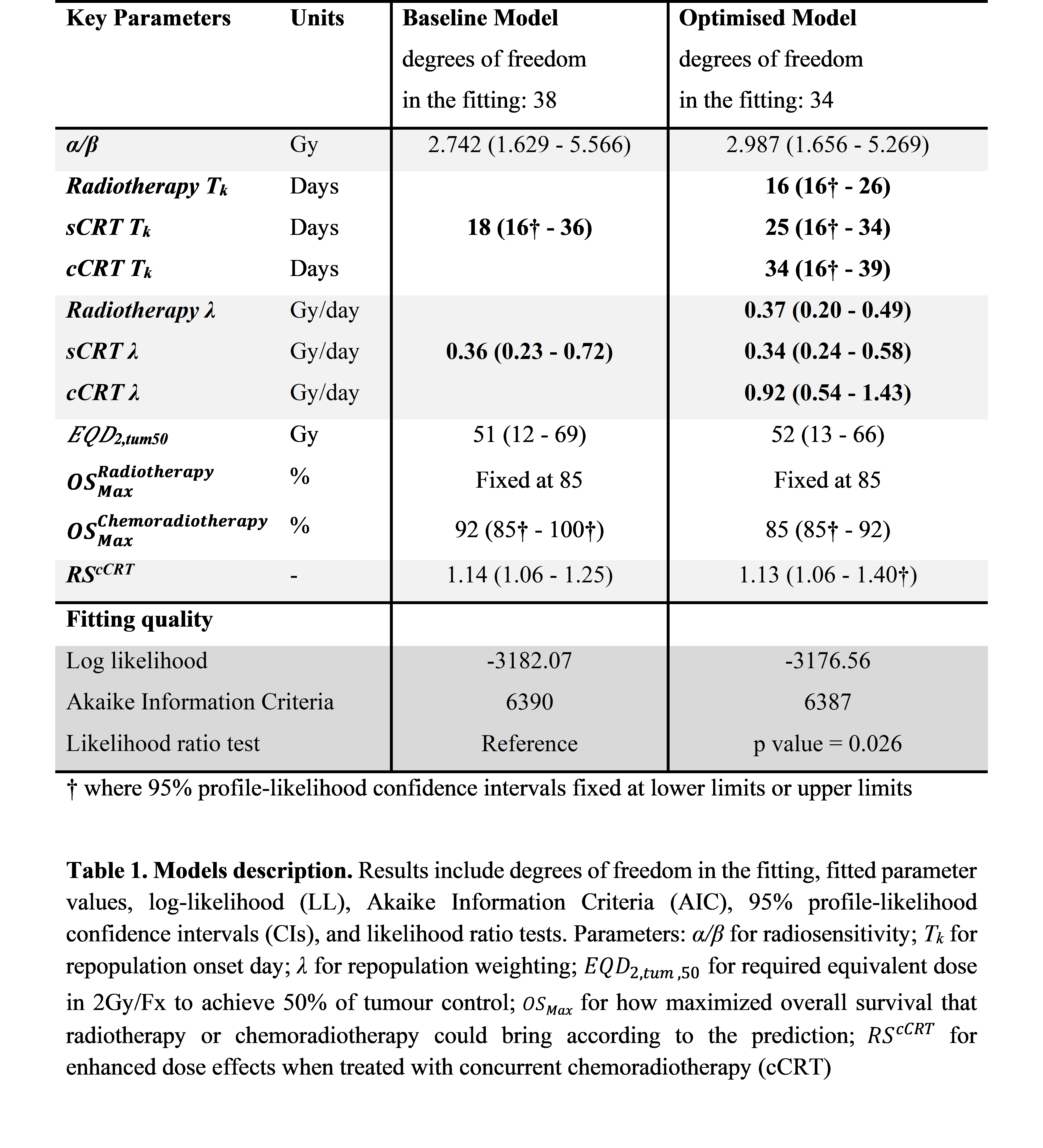
In the baseline tumour
control probability (TCP) model, chemotherapy effects had been included via a
difference in maximum overall survival (OSMax_by Treatment) between radiotherapy and any form of chemoradiotherapy, and a radiosensitisation
factor for concurrent chemoradiotherapy (cCRT) (RS_cCRT). In our
improved model, we separated tumour repopulation parameters (λ,
repopulation rate ; Tk, repopulation onset time) by treatment-type
to test for differences in repopulation between radiotherapy alone, sequential
chemoradiotherapy (sCRT), and cCRT. Model fitting was done using maximum-likelihood
estimation, comparing fits using the Akaike Information Criteria and likelihood
ratio test. LA-NSCLC dose-response curves for radiotherapy, sCRT, and cCRT were
plotted for a fixed treatment duration of 40 days.
Results
Population data were
collated from prospective trials and institutional series with >20 cases published
between 2000 – 2016. The data comprised 4866 NSCLC patients receiving
radiotherapy (1192 patients), sCRT (1792 patients), or cCRT (1882 patients),
with doses varying from 1.26Gy/Fx - 3.00Gy/Fx over 16 - 60 days. In the optimised
model, accelerated tumour repopulation began at 16
days for radiotherapy (95% CI:
16 - 26), 25 days for sCRT (95%
CI: 16 - 34), and 34 days (95%
CI: 16 - 39) for cCRT, and
respectively accounted for 0.37Gy (95%
CI: 0.20 - 0.49), 0.34Gy (95% CI: 0.24 - 0.58) and 0.92Gy (95% CI: 0.54 - 1.43)
radiation dose lost per day of treatment protraction.
Conclusion
This analysis suggests that
cCRT leads to delayed but substantially more rapid accelerated tumour
repopulation late in radiotherapy treatments of LA-NSCLC. Consequently, overall
treatment time should be carefully considered when designing such cCRT treatments.
This analysis partly explains the poorer overall survival seen for protracted dose-escalation
schedules such as 74 Gy in 7.5 weeks in the Phase III randomised clinical trial
- RTOG-0617. Based on the modelling results, dose-escalation of LA-NSCLC
cCRT should be limited to 6 weeks to prevent accelerated tumour repopulation.