EPID in vivo dosimetry implementation world-wide: results of an ESTRO survey
OC-0079
Abstract
EPID in vivo dosimetry implementation world-wide: results of an ESTRO survey
Authors: Marco Esposito1, Jeroen B. van de Kamer2, Evy Bossuyt3, Stephen F. Kry4, Dirk Verellen5, Catharine Clark6, Nuria Jornet Sala7
1Azienda Sanitaria USL Toscana Centro, S.C. Fisica Sanitaria Firenze-Empoli, Firenze, Italy; 2The Netherland Cancer Institute, Division of Radiotherapy, Amsterdam, The Netherlands; 3Iridium Netwerk, Radiation Oncology , Antwerp, Belgium; 4M.D. Anderson Cancer Center, Radiation Physics, Houston, USA; 5Iridium Netwerk, Radiation Oncology, Antwerp, Belgium; 6University College Hospital London, Radiotherapy, London, United Kingdom; 7Hostpital de la Santa Creu i Sant Pau, Radiation Physics, Barcelona, Spain
Show Affiliations
Hide Affiliations
Purpose or Objective
In
vivo dosimetry (IVD) is known to be an effective quality assurance method to
detect deviations between prescribed and administrated dose. From the available
IVD systems, the Electronic portal imaging device (EPID) has been shown to have
great potential for large scale acquisitions of in vivo dosimetry (IVD) data.
In recent years, many institutes developed EPID IVD programs with commercial or
homemade software. In this work we investigated the critical aspects and the
effectiveness of the IVD implementation with a focus on EPID based IVD on an international
level.
Material and Methods
An
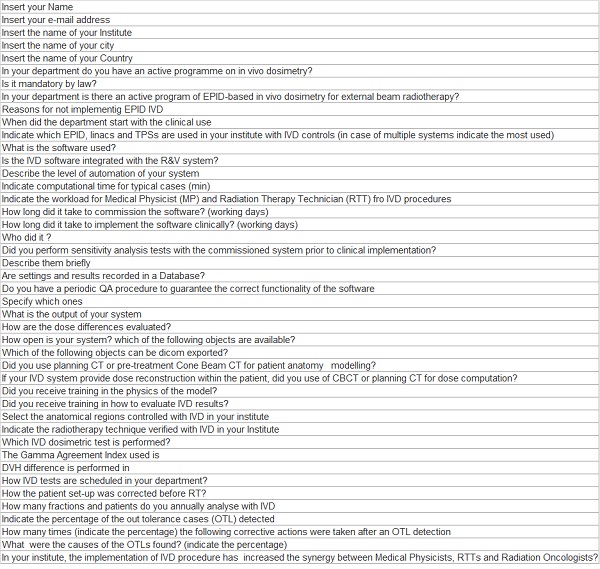
ESTRO working group, created a survey containing 44 questions [Fig1] divided in
three parts: IVD software characteristics, software implementation and data
analysis, and patients results. The survey was sent to the ESTRO mailing list
on 14 October 2019 and was closed on 30 November 2019.
Results
133
institutes participated in the survey, of which 45 used IVD with
EPID. 17 centres submitted statistics of patient IVD data. The software were: Perfraction (SunNuclear) (9), Epigray (DOSISsoft)
(8), Softdiso (Best Medical) (7), Dosimetry Check (LAP) (6), Portal Dosimetry (Varian)
(6), homemade software (6), and IviewDose (Elekta) (3). These in vivo solutions
involve different degrees of automation as well as different metrics for dose
comparison. An average of 2657 patients (range 50-8000) and 10021 fractions (range
200-24000) were annually analyzed with fully
automatic software, compared to 855 patients (range 100-2500) and 2791
fractions (range 1000-6575) with the partially automatic and 266 patients (range
20-1200) and 378 fractions (range 30-3500) with the software without
automation. The percentage of all measurements with results out of institutional
tolerance limits, was, on average, 14% with 10% standard deviation. The
causes of out of tolerance results were: patient anatomical variations
5.2%, setup errors 3.7%, incorrect use of immobilization devices 2%, beam
delivery discrepancies 1.3% and incorrect plan computation 0.3%. Failure of the
IVD algorithm or erroneous EPID acquisitions occurred in 4.5% of fractions. In 2.2%
of fractions, the cause was not unidentified. Sporadic network data transfer
errors were reported by one centre. The actions taken after out of tolerance detection, were, on average: repetition of the IVD test 8.5%, instruction of the
technician for improving the patient setup 3.8%, informing the radiation
oncologist 0.9%, and replanning 1.6%.

Conclusion
In
this study, the degree of global implementation, the high potential to detect
and correct errors, and the challenges for wider spread use of EPID IVD have
been shown. However, the results are very heterogeneous as implementation, data
analysis and underlying causes for out of tolerance are centre dependent. International
guidelines could facilitate harmonization and standardization of EPID IVD use
and facilitate efficient implementation.