The median age at salvage treatment was 71 years (56-85). At
initial diagnosis, 22% presented with low, 66% intermediate, and 13% high risk
localized disease (NCCN). The median time between initial and salvage treatment
was 7 years (3-17). Median PSA prior to
salvage PSA BT was 4.6 (1.2-24), with median PSA doubling time of 15 months
(5-51). Gleason grade group at initial failure was 4 or 5 in 34%, and short
course adjuvant ADT was used in 33%.
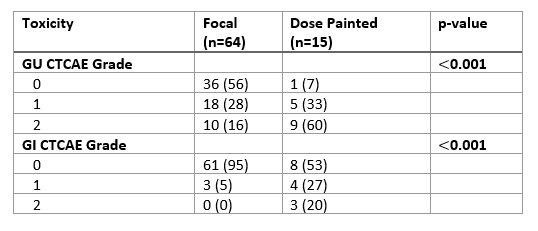
At a median follow up of 38 months (6-134), the 3 and 5 year
FFS (95% CI) rates were 67.8% (56.7-80.9) and 49.1% (35.8 – 67.4) respectively,
with a median time to progression of 59.3 months (42.4-not reached). The 3 and
5 year cumulative incidence of local failure (LF) was 13.9% (95% CI, 4.1-23.7)
and 30.1% (14.6-45.7), respectively. LF occurred earlier in the fBT cohort
(Figure 1), but no statistically significant difference was found (fBT vs.
dpBT, 19% vs. 0% p=0.32 at 3 years, and 27.8% vs. 23.3% at 5 years). The 3 and 5-year cumulative incidence of DM
was 2.9% (0-6.9) and 12.6% (1.2-24), respectively.
There were no G3 toxicity events attributable to
salvage brachytherapy. Overall, grade 2 genitourinary (GU) and gastrointestinal
(GI) toxicity events were reported in 24% and 4% of patients, respectively. The
fBT approach resulted in substantially fewer grade 2 GU and GI toxicity events
compared with the dpBT approach (p<0.001, Table1).
Figure1. Local failure in dpBT and fBT cohorts.
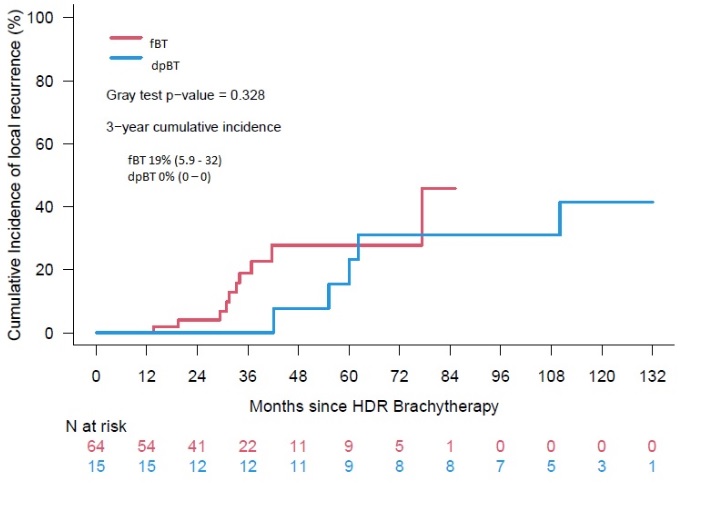
Table1.
Toxicity by Type of Therapy