To
generate the patient specific applicator, a CT scan (Somatom definition edge, Siemens Healthcare GmbH, Germany)
was acquired of the H&N phantom in supine position. Delineation of a CTV in the region of the left nose wing and cheek was
performed by a physician. Next, a 3D mesh of the body and CTV were exported from
Eclipse (Varian, USA) using scripting. Subsequent design of the applicator was done
in TriMatic (Materialise, Belgium). Within a 10 mm thick bolus, nine channels
(2.2 mm diameter) were designed 5 mm from the patient surface and spaced 1 cm
apart from each other. The direction, location and number of
channels were manually optimized for target coverage and minimal local
curvature to assure proper passage of the BT-source. The applicator was printed
on a Raise3D N2+ 3D printer (Raise3D, Netherlands) using PLA (ICE filaments,
Belgium) with 100% infill and 2 shells.
For
treatment planning, a second CT was acquired of the applicator positioned on
the phantom, with 5f BT catheters and radio-opaque markers in place. Next, the dosimetric
planning was performed in Oncentra Brachy 4.5.2 (Elekta, Netherlands) with a 7
Gy prescription at 5 mm under the body surface.
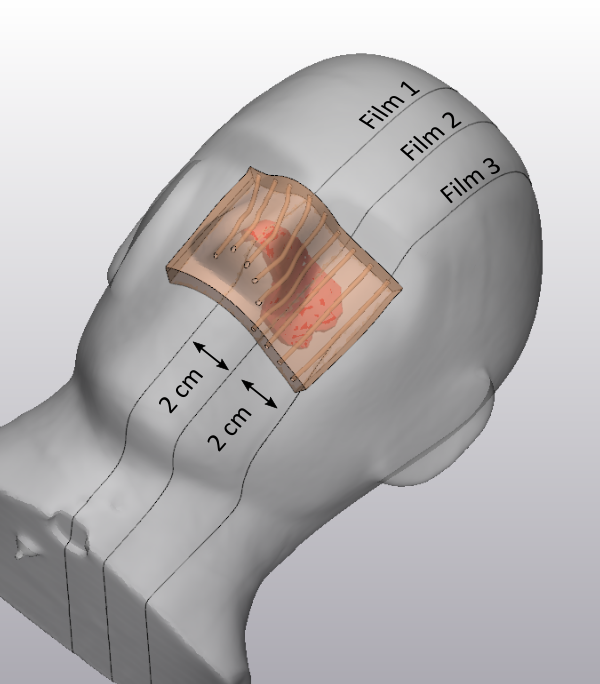
The treatment
was delivered with an Ir-192 Flexitron afterloader (Elekta, Netherlands) with
laser cut EBT3 films positioned in the three sagittal planes of the phantom. The films were
scanned and converted to dose using a calibration procedure for page-sized
films and triple channel correction methodology1.