Freiburg Flap Surface Applicator Brachytherapy positional accuracy on MR-only PETRA images
OC-0020
Abstract
Freiburg Flap Surface Applicator Brachytherapy positional accuracy on MR-only PETRA images
Authors: Evangelia Kaza1, Casey Y. Lee1, Robert A. Cormack1, Phillip M. Devlin1, Ivan Buzurovic1
1Brigham and Women’s Hospital, Dana-Farber Cancer Institute, Harvard Medical School, Radiation Oncology, Boston, USA
Show Affiliations
Hide Affiliations
Purpose or Objective
For MR-only treatment planning in skin High Dose Rate (HDR) surface
applicator brachytherapy (SABT) it is crucial to detect applicator channels on
MRI with high spatial accuracy. An optimized PETRA (Pointwise Encoding Time Reduction
with Radial Acquisition) MR sequence has shown the potential to visualize
Freiburg Flap (FF) applicators for skin SABT. This study aimed to develop an
algorithm to automatically detect FF applicator catheters on PETRA images and estimate
their positional accuracy by comparing calculated distances between them to their
known distances in a FF.
Material and Methods
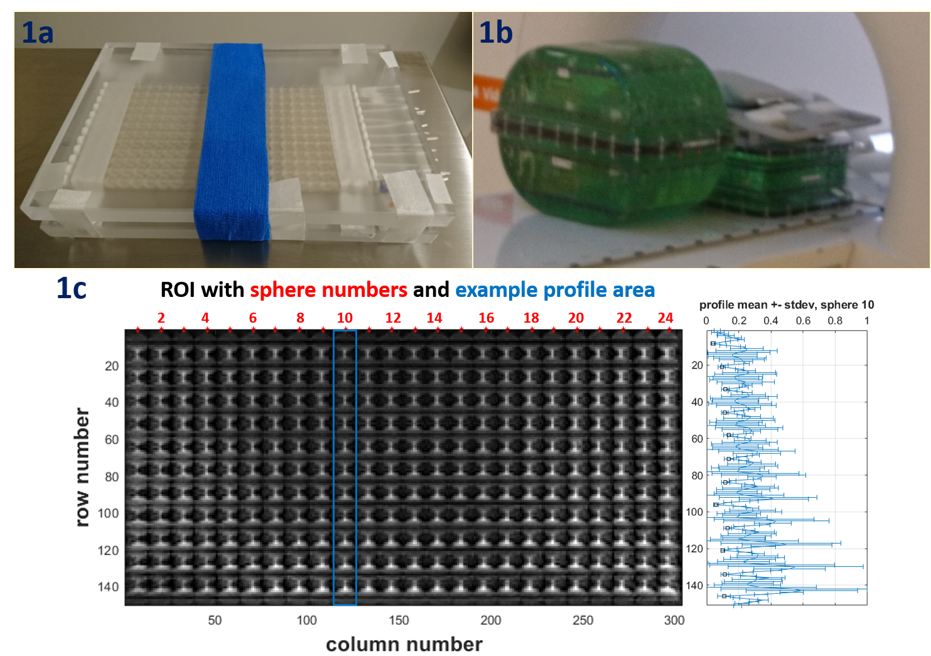
An FF
applicator (12 catheters, each passing through the center of 24 spheres with
10mm diameter) was fixed between two plexiglass blocks with its sides parallel
to the block edges and placed on a flat MagPhan TMR008 phantom in a 3T Siemens
Vida scanner (Fig1 a, b). Coronal and axial 3D PETRA images (TR\TE\TI
3.3\0.07\100 ms, FOV 280x280 mm2, 0.8 mm isotropic voxels, BW 406
Hz/px) were acquired using a top UltraFlex Large 18 and bottom Spine 32 coil.
A custom
MATLAB code selected a ROI comprising the FF in the coronal plane. The central column
of the top left sphere was manually selected, and the central column position of
top row reference spheres (RSs) to its right was estimated using pixel size. Row
profiles of 13 columns corresponding to each RS were extracted and normalized
and their numerical gradient was computed. Profile mean and standard deviation
and gradient mean over columns were calculated for each RS (Fig 1c). Catheter
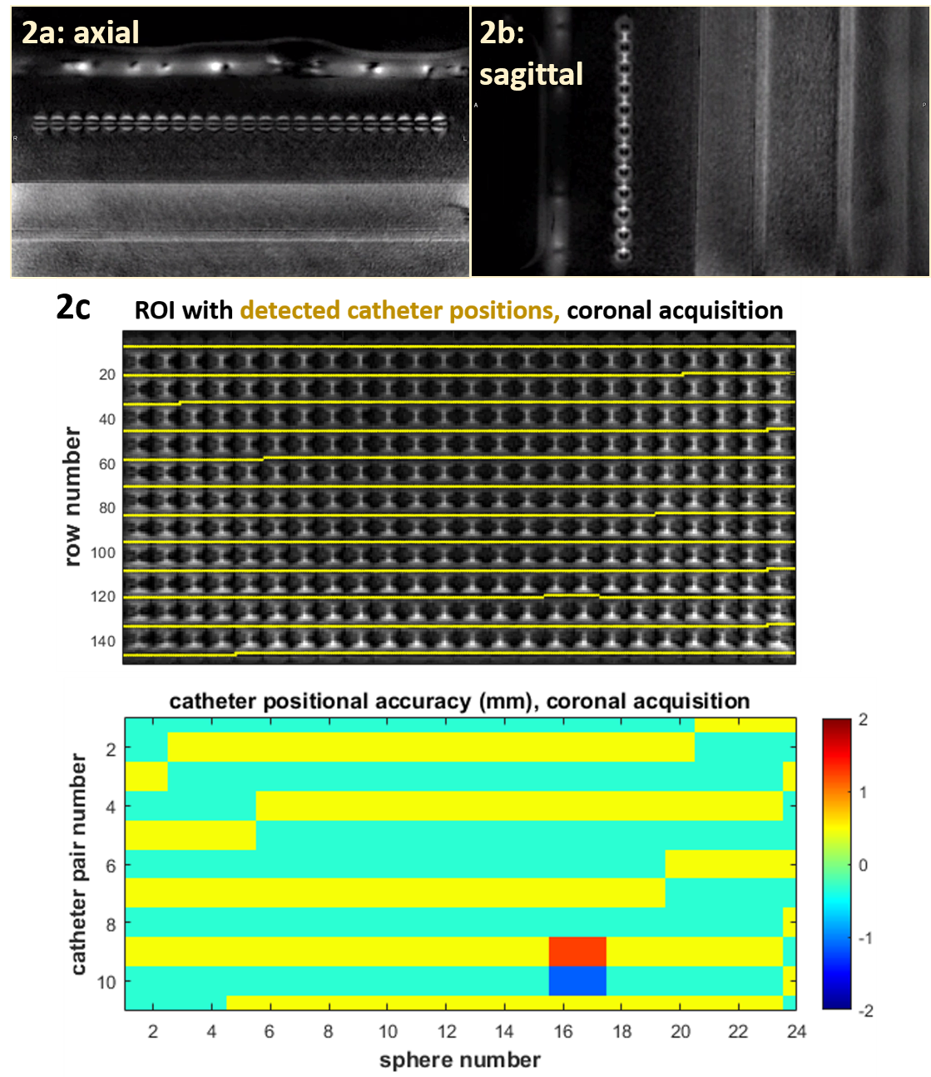
positions were defined as row numbers corresponding to minima of profile mean over
rows, found within 2 pixels of minima of standard deviation and of gradient
mean. The distance between adjacent catheters was calculated from their row
difference. Catheter distance difference from the known 10 mm value yielded
positional accuracy. Average absolute positional accuracy and its standard
deviation were calculated for all adjacent catheter pairs of each RS in a ROI
(Fig 2c).
Results
Catheters inside
the FF were distinguished on PETRA images in all 3 orientations with higher
signal intensity than air and lower signal intensity than silicone spheres (Fig
1 c; Fig 2 a, b). Automated catheter detection in the coronally placed
applicator was feasible using the proposed algorithm for originally acquired
and for reconstructed coronal slices centered on the applicator. The positional accuracy obtained was 0.40 ± 0.11 and 0.52 ± 0.30 for two acquired, and
0.46 ±
0.23 and 0.53 ± 0.30 (average ± standard deviation) for two
reconstructed coronal slices encompassing the catheters.
Conclusion
The
catheters of an FF applicator with known dimensions were detected on PETRA MR
images using a novel algorithm. Overall catheter positional accuracy was around
half millimeter, indicating reliable detection of catheters along their length
inside the applicator. These results suggest that PETRA provides adequate
catheter detection accuracy for application in SABT MR-only treatment planning.