Stereotactic Body Radiation Therapy for oligorecurrent thymoma: a monocentric experience
PO-1500
Abstract
Stereotactic Body Radiation Therapy for oligorecurrent thymoma: a monocentric experience
Authors: Matteo Sepulcri1, Chiara Paronetto1, Valeria Santoro1, Anna Gorza1, Francesca Gessoni1, Alessandro Scaggion2, Marco Fusella2, Marco Muraro1
1Veneto Institute of Oncology IOV-IRCCS, Radiation Oncology, Padua, Italy; 2Veneto Institute of Oncology IOV-IRCCS, Medical Physics, Padua, Italy
Show Affiliations
Hide Affiliations
Purpose or Objective
Thymic malignancies are rare entities. Due to the lack of published data, there is no strong evidence available for the best management of recurrent thymoma. Despite radical surgery, the recurrence rates range between 10% and 30%. The most common thymoma’s metastatic sites are the pleura and the lungs; the treatment of the oligometastatic disease is usually surgical when feasible, while chemotherapy is preferred in case of a polimetastatic disease. In this setting radiotherapy has been historically reserved for symptoms palliation, but the development of SBRT allows a further line of treatment for oligometastatic patients who either refuse surgery or are not eligible for it. The purpose of this study was to examine the disease local control (LC) and acute toxicities following SBRT.
Material and Methods
From November 2018 to December 2020, 9 patients for a total of 16 thymoma metastases have been treated in our centre using a FFF-RapidArc with 6MV and daily kV-CBCT. All of the patients underwent surgery for the primary tumor with or without neoadjuvant chemotherapy, followed by adjuvant RT except in one case. The best approach for all the recurrences was discussed at a multidisciplinary board. The patients characteristics are listed in the table below.
CASE | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 |
AGE | 85 | 50 | 29 | 70 | 58 | 58 | 70 | 50 | 55 |
SEX | F | M | F | F | M | F | M | M | M |
HISTOLOGY | B1 | B1 | B1 | B1/2 | B1 | B2 | B1 | B1 | B2/3 |
MASAOKA STAGE | IVB | IVA | IIB | IIIB | III | IVA | IVA | IIIA | IVA |
NEOADJ CT (Etoposide, Cisplatin, Epirubicin) | - | x4 | x4 | x3 | - | x6 | - | x3 | x3 |
SURGERY (month/year) | 11/ 2014 | 11/ 2010 | 05/ 2015 | 07/ 2017 | 08/ 2013 | 07/ 2012 | 09/ 1998 | 01/ 2018 | 03/ 2016 |
ADJ RT (Gy/fr) | 50.4/28 | 50.4/28 | 54/27 | 50/25 | 25/5 | 54/27 | 50/25 | - | 50/25 |
PREVIOUS THERAPY FOR RELAPSE | Yes | No | No | Yes | Yes | Yes | Yes | Yes | Yes |
Results
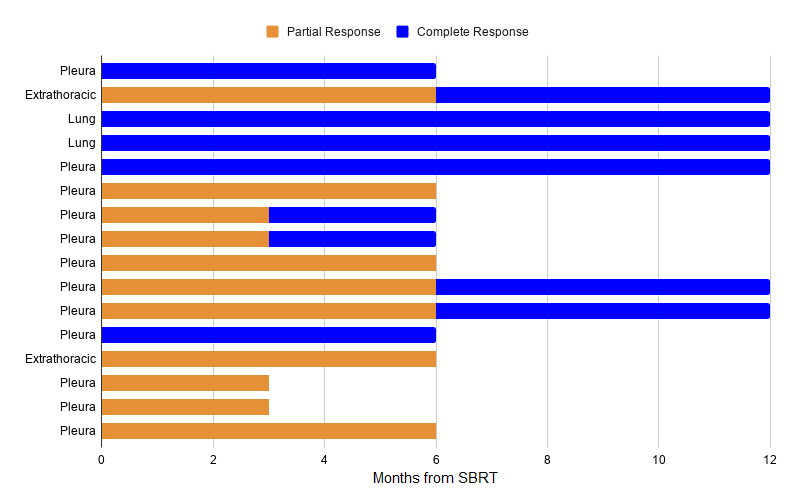
The majority of the lesions were located in the pleura (75%), the remaining in the lungs (12.5%) or extrathoracic sites (12.5%). The mean PTV volume and diameter were respectively 26.3 cc and 3.12 cm. The SBRT treatment was delivered in 5 fractions in all cases; the mean dose was 33.75 Gy (range 30-40), and mean BED10Gy was 58.5 Gy (range 48-72). The median follow up was 12 months (4-27). No relapse in the RT field was recorded. Three of the nine patients developed secondary pleural lesions, two of whom underwent a second SBRT session. The treatments were well tolerated, there were no acute or late toxicities due to SBRT. At the present day the local control of the treated lesions is 100%; in particular at 3 months 31,25% patients achieved a complete response (CR), 62,5% a partial response (PR), while in 6,25% of the cases the disease remained stable; at 6 months, CR and PR were reached in a rate of 56.25% and 43.75%, respectively. After 12 months, CR was recorded for 89% of the patients.
Conclusion
Based on our data, SBRT might be a valid approach for recurrent thymoma due to its intrinsic radiosensitivity, overall safety, excellent local disease control and viability for multiple lesions simultaneously. Further studies need to be conducted to establish the role of SBRT for oligorecurrent thymomas.