Feasibility of stereotactic body radiotherapy of (ultra)central lung tumors using an 1.5 T MR-linac
Laura Merckel,
The Netherlands
PO-1161
Abstract
Feasibility of stereotactic body radiotherapy of (ultra)central lung tumors using an 1.5 T MR-linac
Authors: Laura Merckel1, Sara Hackett1, Astrid van Lier1, Madelon van den Dobbelsteen1, Marnix Rasing1, Louk Snoeren1, Corine van Es1, Martin Fast1, Peter van Rossum1, Joost Verhoeff1
1UMC Utrecht, Radiation Oncology, Utrecht, The Netherlands
Show Affiliations
Hide Affiliations
Purpose or Objective
SBRT is an
important modality for the radical treatment of malignant tumors in the lungs. Treatment with highly ablative doses in central or ultracentral tumors has been demonstrated to
result in high rates of toxicity. MRI-guidance during treatment with daily plan
adaptation may aid accurate delineation of OARs and target volumes in proximity
of the mediastinum with daily plan adaptation allowing for safer treatment. In
this study, we report the first clinical experiences on the safety and feasibility
of SBRT of (ultra)central lung tumors on an 1.5 T MR-linac.
Material and Methods
Both
patients with primary NSCLC and patients with an oligoprogressive metastatic
lung nodule or mediastinal lymph node were eligible for treatment on the Unity
MR-linac (Elekta AB, Stockholm, SE) if their PTV was within 2 cm of the mediastinum.
Pre-treatment imaging with 4D-CT and MRI was performed in treatment position
and a pre-treatment offline IMRT plan was created in Monaco v5.40.01. Patients
were treated to a stereotactic dose of 60 Gy in 8 or 12 fractions. An in-house
developed T2-weighted 3D sequence acquired during free breathing was used for
online delineation and treatment planning. For each fraction, contours of ITV
and OARs were propagated using deformable image registration. A radiation
oncologist modified the contours of ITV and relevant OARs and a new IMRT plan
was created.
Results
Ten
patients were treated and completed all of their planned 104 fractions on the
MR-linac. The median duration of treatment was 41 minutes (range 32-70 minutes)
with a median beam-on time of 8.9 minutes (Figure 1). No grade ≥3 acute toxicity
was observed. In 2 patients, a significant decrease in ITV size of 58% and 37% was
observed due to tumor shrinkage during treatment (Figure 2). In the other
patients, the majority (81%) of online ITVs were within ±15% of the fraction 1 volume. Compared to the offline treatment plan,
ITV coverage of the online plan was similar in 52%, better in 34% and worse in
14% of fractions. Reduced coverage was associated with preferentially meeting
OAR constraints.
Figure 1.
Pie-chart demonstrating the different steps and respective average durations of
the MR-guided online workflow.
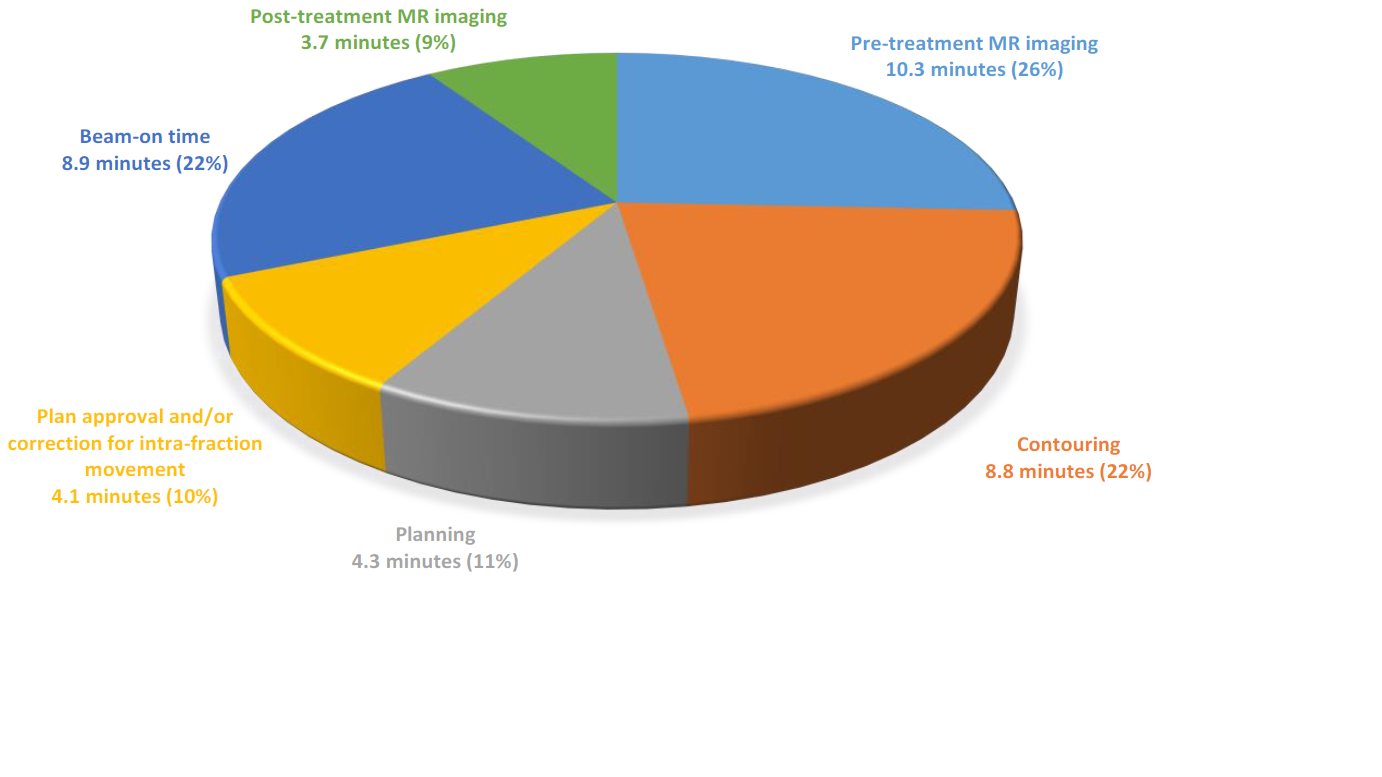
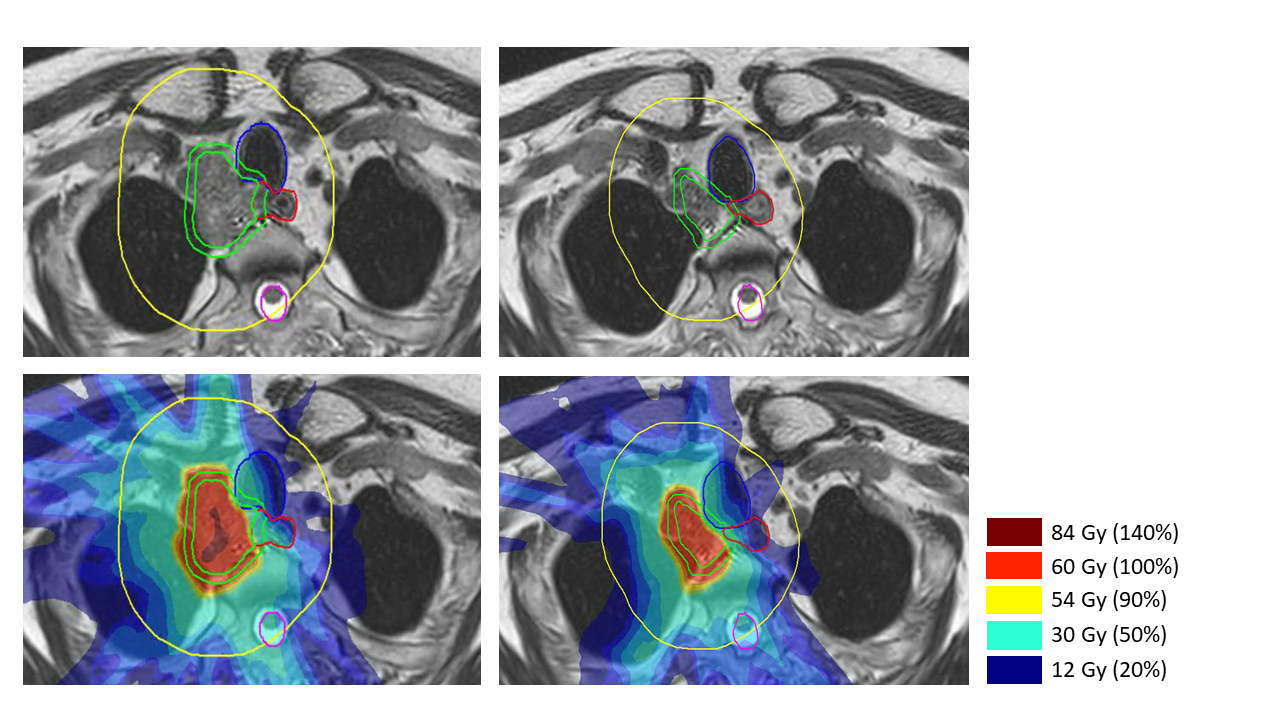
Figure 2. Online
MRI and dose distribution of the 1st (left) and 12th
(right) fraction of a patient with a mediastinal lymph node metastasis of a SCLC
in whom a 58% decrease in ITV was observed during treatment. The ITV (green) and
OARs (esophagus (red), trachea (blue), spinal cord (purple)) within a 3 cm ring
(yellow) around the PTV (green) are modified during treatment by a radiation oncologist.
Conclusion
We demonstrate
the safety and feasibility of SBRT of (ultra)central lung tumors on an 1.5 T
MR-Linac. All patients completed all treatment fractions on the MR-linac with improved
ITV coverage in 34% of fractions through daily plan adaptation. In 2 patients,
a significant decrease in ITV size was observed during treatment, illustrating
the additional benefits of MRI-guided radiotherapy.