121 SRS cases (85 single and 36 multiple target) with
280 couch kicks in total were evaluated. For 66.8 % of couch kicks the
specified tolerances were exceeded and patient position had to be corrected.
Intra-fractional translational
errors (one standard deviation [SD]) were 0.50 vs. 0.22 mm in left-right, 0.46
vs. 0.22 mm in superior-inferior, and 0.37 vs. 0.21 mm in anterior-posterior
direction (see figure), with a mean three-dimensional vector of 0.71 vs. 0.33
mm [without versus with positioning readjustment after couch kick].
Furthermore, rotational errors
were 0.43 vs. 0.28° in pitch, 0.37 vs. 0.25° in roll, and 0.34 vs. 0.19° in yaw
rotation.
Finally, the change in dose
distribution due to uncorrected 6D errors was calculated to assess the effect
on target coverage.
A few single target (9 %) and almost
all single-isocenter multiple target cases (91 %) would be clinically
unacceptable (coverage loss >5 %) if the positioning readjustment
had not been applied. The mean lesion size was 1 cc (SD 0.9 cc) and the average
PTV-center to isocenter distance for multiple targets was 4.8 cm (SD 1.7 cm).
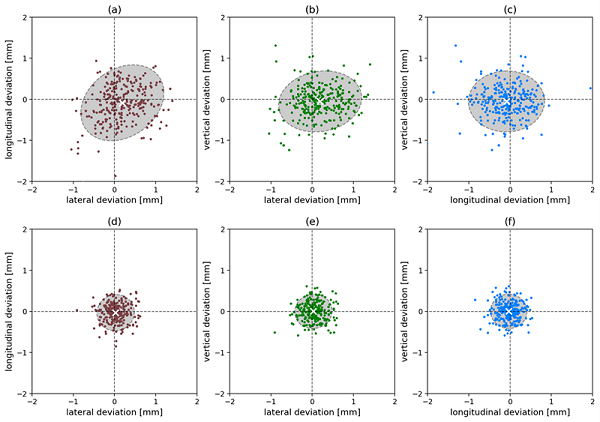
Scatter plots with mean and 95% confidence regions of translational positioning
shifts for all 280 couch kicks: uncorrected (a-c) and corrected (d-f) resulting
in tolerable deviations (0.5 mm, 0.5°)