Commissioning HyperArc for Single Targets including Benign Tumours
Daniel Egleston,
United Kingdom
PO-1904
Abstract
Commissioning HyperArc for Single Targets including Benign Tumours
Authors: Daniel Egleston1, Robert Brass1
1The Clatterbridge Cancer Centre, Physics, Liverpool, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
To show
HyperArc™ plans have equivalent or improved plan quality compared to
RapidArc™ VMAT, for SRS treatment of brain metastases, meningiomas,
and acoustic neuromas, with the overall goal of commissioning HyperArc™ treatments for single cranial targets.
Material and Methods
8 patients who had previously received non-coplanar RapidArc™
VMAT for single targets on a Varian Novalis Tx linac were replanned
using HyperArc™ for treatment on a Varian Edge linac.
The patients represented a range of sites within the
skull, constituting 4 brain metastases, 2 acoustic neuromas, and 2 meningiomas.
4 plans had isocentres within the central patient protection zone, and were
planned with both full arc geometry using the standard 5 half-arcs and reduced arc geometry using 4 half-arcs excluding the central arc as in Figure 1. The
other 4 had lateral isocentres, and were planned with reduced arc geometry of 4 half-arcs excluding the contra-lateral arc. 1 brain
metastasis and 1 meningioma patient additionally had some
overlap of the PTV with brainstem. Plan quality was compared to the
previous RapidArc™ VMAT plan. The effects of normalising to deliver 80% dose to 99% of the PTV were additionally
investigated. Each HyperArc™ plan was verified by analysis with
both PDIP and Octavius, and analysed by DoseCHECK™ independent
dose calculation.
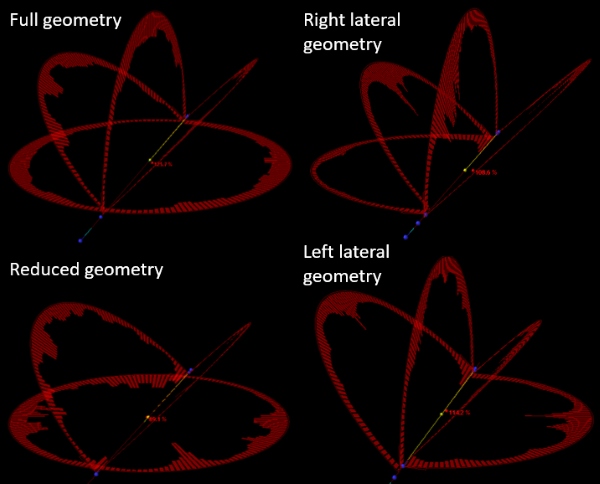
Figure 1: Diagram of HyperArc™ arc geometries.
Results
HyperArc™ plans meeting local OAR constraints and plan quality
tolerances were created for all 8 patients. The Conformity Index was equal to
or lower than the RapidArc™ VMAT plan in all cases. However,
normalising the HyperArc™ plans to deliver 80% dose to 99%
of the PTV improved the visual conformity. The D0.1cc to the PTV was
below 110% for all plans except one brain metastasis
plan, supporting a change in local protocol to restrict hotspots to 110% for
benign targets. There was no discernible difference in plan quality using
reduced 4 half-arc geometry compared to full 5 half-arc geometry.
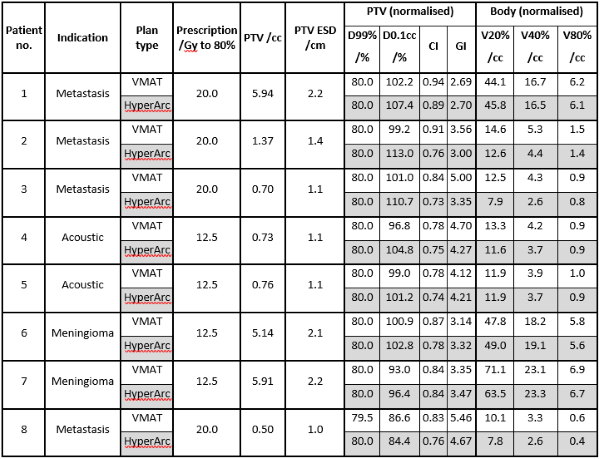
Figure 2: Table comparing dosimetric and volumetric results for normalised plans.
All
PDIP analyses passed at 3%/2mm, with a low dose
threshold of 20% and 95% gamma passing threshold. Only one plan failed Octavius analysis using the same criteria as PDIP, and passed using a reduced VOI to discount low dose gamma failures far from the PTV. All but one plan passed DoseCHECK™ analysis at 3%/1mm, with a 20% low dose threshold and
95% gamma passing rate. As the failed plan had PTV abutting bone, differences in dose modelling across the density interface reasonably
increased the failure rate. This plan passed after recalculating at 4%/1mm
criteria.
Conclusion
HyperArc™ is suitable for single-target SRS
treatments for brain metastases, meningiomas, and acoustic neuromas, using reduced
four arc geometries and normalising the prescription dose to 99% of the PTV as
standard. The results justify restricting hotspots to 110% for benign targets. DoseCHECK™, PDIP, and Octavius analysis verify dosimetric accuracy and plan
deliverability.