Optimising splenic dose with PBT and VMAT for distal oesophageal cancer
Owen Nicholas,
United Kingdom
PO-1241
Abstract
Optimising splenic dose with PBT and VMAT for distal oesophageal cancer
Authors: Owen Nicholas1, Agelos Saplaouros2, Jamil Lambert2, Greg Fegan3, Richard Hugtenburg4, Sarah Gwynne1
1South West Wales Cancer Centre, Oncology, Swansea, United Kingdom; 2Rutherford Cancer Centres, Radiotherapy Physics, Newport, United Kingdom; 3Swansea University, Swansea Trials Unit, Swansea, United Kingdom; 4Swansea University, Medical Physics, Swansea, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
Higher rates of G4 lymphopenia is predictive of poorer
survival in oesophageal cancer (OEC). Previous work has found a dose dependant
relationship between mean splenic dose (MSD) and absolute lymphocyte count. In distal
OECs, the spleen often receives significant doses due to its proximity to the
target volume (TV) but is often not considered during RT planning. PBT’s superior
physical properties may reduce splenic dose compared to photon RT. Aims: 1) Ascertain
feasibility of reducing dose to the spleen in lower OEC with PBT and VMAT,
while meeting dose constraints to other OARs. 2) Test
spleen constraints used during optimisation of PBT and VMAT plans, that may be
used in future trial protocols and clinical practice. 3) Quantify
any dosimetric advantages to the spleen, if present, of PBT over VMAT
Material and Methods
Twenty distal OEC cases from the UK NeoSCOPE trial were used.
In addition to the quality-assured clinical TVs and OARs, the whole spleen was
outlined as per RTOG guidance in each case. Nominal PBT plans were robustly
optimised with and without spleen dose constraints. VMAT plans were created
with spleen constraints for comparison. All plans were created on Pinnacle
(Philips; PBT – v14, VMAT – v16.2) to a dose of 45Gy/25#. For TV coverage and OARs, NeoSCOPE trial dose
constraints were used. Novel whole spleen constraints used were taken from previous
work in pancreatic cancer. These were MSD <4.5GY (optimal), V10Gy <12%
(optimal), MSD <10Gy (mandatory) and V15 <20% (mandatory). A 3-beam
arrangement with gantry angles of 135°, 180° and 225° were used for all PBT
plans. The statistics for PBT plans with and without spleen optimisation were
compared. PBT (spleen-optimised) plans were also compared to VMAT
(spleen-optimised) plans. Paired t-test (two-tail) were performed for each
tested DVH parameter to assess for significance (P < 0.05).
Results
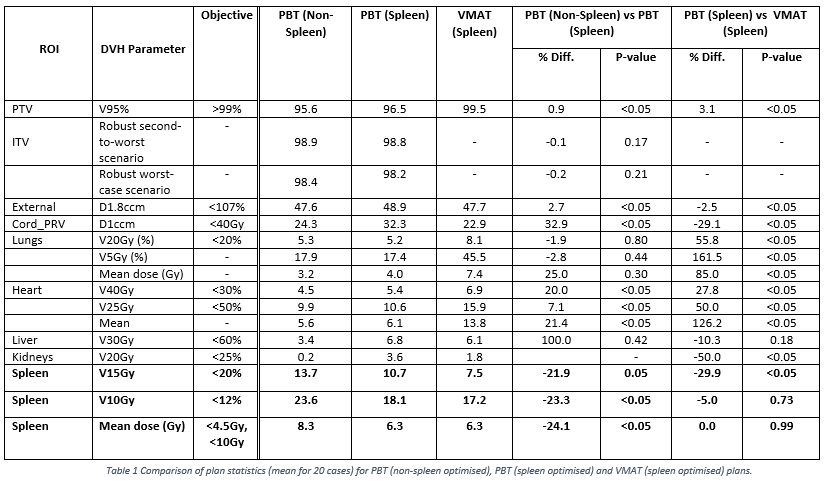
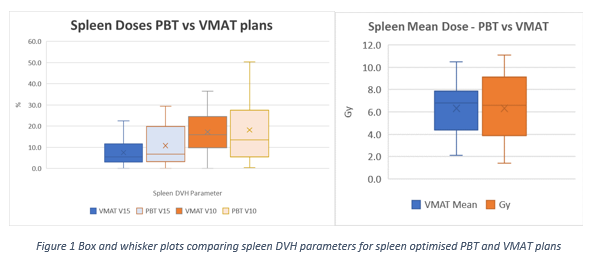
Full results are detailed in Table 1 and Figure 1.
Conclusion
This study demonstrates that, at a dose level of 45Gy/25#, it
is feasible to incorporate spleen constraints while meeting other planning
goals for distal OEC. Spleen optimised cases had higher cord, heart and liver
doses although differences are small and may not be clinically significant. PBT
plans resulted in comparable MSD compared to VMAT. However, there was wider variation
in splenic dose for PBT suggesting a greater sensitivity to individual patient
anatomy. In most cases (PBT and VMAT) mandatory constraints were met but for
most plans, optimal constraints were exceeded. A greater proportion of VMAT
plans met all constraints.
VMAT may achieve greater spleen sparing in distal OEC compared
to PBT. However, a lower integral dose with PBT may still result in lower rates
of G4 lymphopenia. MSD of <10Gy is a feasible optimal constraint for
clinical use. Prospective studies are required to ascertain the impact on
splenic irradiation on G4 lymphopenia rates and survival outcomes.