Cochlea sparing optimized radiotherapy for nasopharyngeal carcinoma
PO-1020
Abstract
Cochlea sparing optimized radiotherapy for nasopharyngeal carcinoma
Authors: Erwin Vu1, Enkelejda Lamaj1, Janita van Timmeren1, Chiara Leonardi1, Izabela Pytko1, Louise Marc1, Matthias Guckenberger1, Panagiotis Balermpas1
1University Hospital Zurich, Radiation Oncology, Zurich, Switzerland
Show Affiliations
Hide Affiliations
Purpose or Objective
Definitive chemoradiotherapy (CRT) is standard of care for nasopharyngeal carcinoma. Due to the tumor localization and concomitant platinum-based chemotherapy, hearing impairment is a frequent complication, without defined dose-threshold. The widely accepted QUANTEC constraint for the cochlear tolerance dose of 45 Gy is associated with an expected complication rate of <30%. In this study, we aimed to achieve the maximum possible cochleae sparing.
Material and Methods
Treatment plans of 20 patients, treated with CRT (6 IMRT and 14 VMAT) based on the QUANTEC organs-at-risk constraints were investigated. The cochleae were re-delineated independently by two radiation oncologists, whereas target volumes and other organs at risk (OARs) were not changed. The initial plans, aiming to a mean cochlea dose <45 Gy, were re-optimized with VMAT, using 2-2.5 arcs without compromising the dose coverage of the target volume. Mean cochlea dose, PTV coverage, Homogeneity Index (HI), Conformity Index (CI) and dose to other OAR were compared to the reference plans. NTCP models were performed for tinnitus and hearing loss. Wilcoxon signed-rank test was used to evaluate differences, a p-value <0.05 was considered significant.
Results
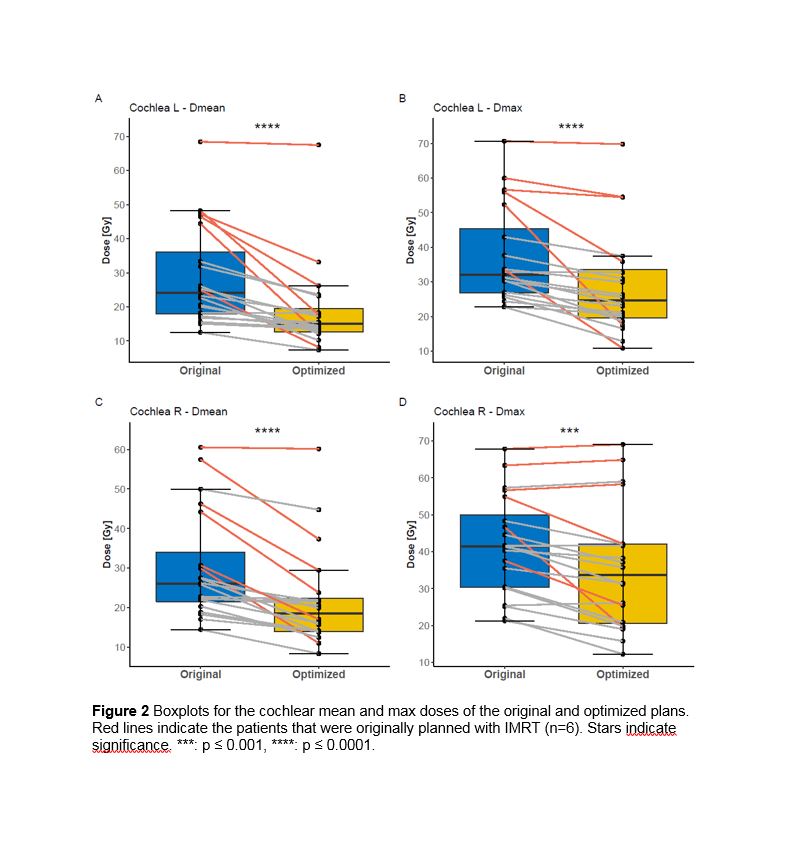
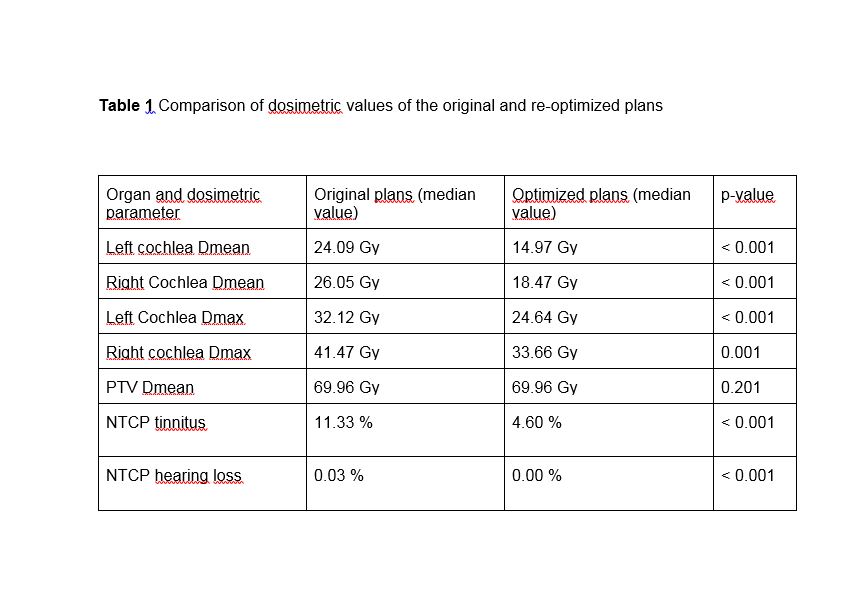
The re-optimized plans achieved a statistically significant lower dose for both cochleae (median dose for left and right 14.97 Gy and 18.47 Gy vs. 24.09 Gy and 26.05 Gy respectively, p<0.001) compared to the reference plans, without compromising other plan quality parameters. The median NTCP for tinnitus of the most exposed sites was 11.3% (range: 3.52 – 91.1%) for the original plans, compared to 4.60% (range: 1.46 – 90.1%) for the re-optimized plans (p<0.001). For hearing loss, the median NTCP of the most exposed sites could be improved from 0.03% (range: 0 – 99.0%) to 0.00% (range: 0 – 98.5%, p<0.001).
Conclusion
A significantly improved cochlea sparing beyond current QUANTEC constraints is feasible without compromising the PTV dose coverage in nasopharyngeal carcinoma patients treated with VMAT. Based on NTCP analyses, such an exposure would reduce the probability of both tinnitus and hearing loss significantly. Not a single quality parameter was inferior in the cochlea-optimized plans, while the median number of monitor units and the beam-on time of the optimized plans were reasonable. These findings highlight the practicability of intensive cochlea sparing for daily routine. As there appears to be no threshold for hearing toxicity after CRT, this should be considered for future treatment planning. The clinical effect of this optimization should be evaluated in the future prospective trials.