Single-Fraction versus Double-Fraction HDR boost for high-risk prostate cancer: long-term outcomes
PH-0657
Abstract
Single-Fraction versus Double-Fraction HDR boost for high-risk prostate cancer: long-term outcomes
Authors: Alai Goñi Ramirez1, Belen De Paula Carranza1, Pablo Fernández Gonzalo2, Eva María Sáenz de Urturi1, Nuria Bultó Boqué1, Mikel Egiguren Bastida2, María Pagola1, David Ignacio Ortiz de Urbina1, Daniel Roura1, Jon Belloso3, Gregorio Garmendia3, Arancha Ayete Andreu4, Vicent Pastor Sanchis5, Albert Bartrés Salido6, Noelia Suarez5, Melanie Erzilbengoa6, Jesús Rosa Nieto1
1Fundación Onkologikoa - UGC Oncología Gipuzkoa, Radiation Oncology, San Sebastian, Spain; 2Fundación Onkologikoa - UGC Oncología Gipuzkoa, Radiation Oncology, San Sebastián, Spain; 3Hospital Universitario Donostia, Urology, San Sebastian, Spain; 4V, Radiation Oncology, San Sebastian, Spain; 5Fundación Onkologikoa - UGC Oncología Gipuzkoa, Medical Physics, San Sebastian, Spain; 6Fundación Onkologikoa - UGC Oncología Gipuzkoa, Medical physics, San Sebastian, Spain
Show Affiliations
Hide Affiliations
Purpose or Objective
To
determinate and compare long-term biochemical control rates, survival and
toxicity outcomes between high-dose-rate brachytherapy (HDR-BT) boost schemes
(single 15Gy fraction versus double 9.5Gy fraction) in treatment of high-risk
prostate cancer patients.
Material and Methods
Between january-2007 and december-2017, 361 patients with high-risk prostate cancer were treated in our institution with external beam radiotherapy (EBRT) plus CT-based iridium192 HDR-BT boost; either with 15Gy single fraction (15Gy-BT) boost or with double 9.5Gy fraction (2x9.5Gy-BT) boost administered 6 hours apart in a single implant. All patients received EBRT 46Gy in 23 fractions of pelvic irradiation encompassing the prostate and seminal vesicles after HDR-BT boost. Those with less than 3-year follow-up and less than 3 post treatment prostate-specific antigen (PSA) were excluded. Clinical outcomes and toxicity were evaluated and compared in these BT boost schemes. Toxicity was evaluated using Common Terminology Criteria for Adverse Events (CTCAE) version 5.0.
Results
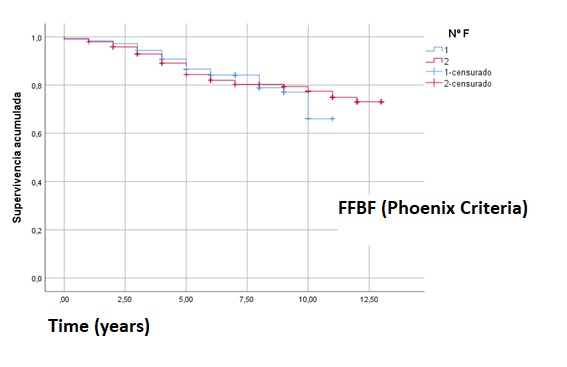
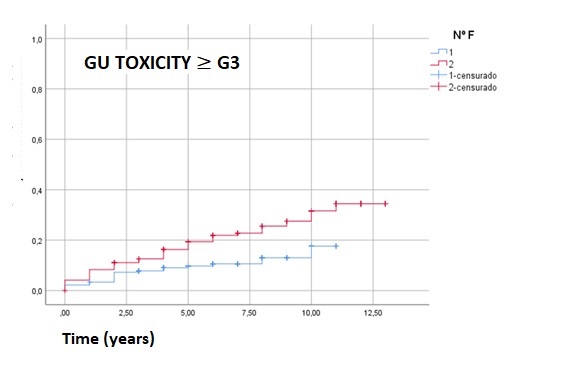
About 325 from 361 patients satisfied inclusion criteria; 180 treated with 15Gy-BT boost and 145 treated with 2x9.5Gy-BT boost. The median follow-up was 7 years for the 15Gy-BT cohort and 11 years for the 2x9.5Gy-BT cohort. Median age was 70 years (range: 47-83) for both cohorts and 91.8% of patients received androgen deprivation therapy (ADT). Freedom from biochemical failure (FFBF) defined by Phoenix-criteria was 87.8% at 5 years and 82.2% at 10 years in 15Gy-BT group, and 88.5% and 80% at 5 and 10 years in 2x9.5Gy-BT group, respectively. Similarly, there was no statistical significant difference in metastasis free survival (MFS) at 5 and 10 years; 93.9% and 91.1% for 15Gy-BT group and 94.5% and 87.6% for 2x9.5Gy-BT group, respectively. There was no difference in overall survival (OS) at 10 years between schemes; 84.6% and 66.9% for the 15Gy-BT group and the 2x9.5Gy-BT group, respectively. Six months after treatment, genitourinary (GU) grade 3 or higher toxicity was 2.2% in the 15Gy-BT group and 4.1% in the 2x9.5Gy-BT group, with no grade 3 or higher acute gastrointestinal (GI) toxicity in both groups. GU grade 3 or higher late toxicity was statistically unfavorable for 2x9.5Gy-BT cohort: 9.4% and 11.7% at 5 and 10 years in 15Gy-BT group, and 18,6% and 27,6% at 5 and 10 years in 2x9.5Gy-BT group, respectively. No significant difference was found in GI grade 3 or higher late toxicity: 1.7% for both 5 and 10 years in the 15Gy-BT group and 0.7% at 5 years and 2.1% at 10 years in the 2x9.5Gy-BT group, respectively.
Conclusion
Although both 15Gy-BT and 2x9.5Gy-BT boost schemas achieve excellent long-term biochemical and survival rates in combination with EBRT for high-risk prostate cancer, late grade 3 GU toxicity was statistically unfavorable for 2x9.5Gy-BT boost. No differences in acute GU and GI toxicity were observed between schemas. Late grade 3 or higher GI toxicity was similar in both groups.