Starting a new era in radiotherapy, transition of work from radiation-oncologist to RTT.
PH-0159
Abstract
Starting a new era in radiotherapy, transition of work from radiation-oncologist to RTT.
Authors: Liselotte ten Asbroek1, Lisanne Zwart1, Erik van Dieren1, Francisca Ong1, Elisabeth de Wit1
1Medisch Spectrum Twente, Radiotherapy, Enschede, The Netherlands
Show Affiliations
Hide Affiliations
Purpose or Objective
CBCT-guided online adaptive radiotherapy has been
introduced as a standard treatment for all our prostate cancer patients and is
supervised by either a radiation-oncologist (first four fractions) or an
advanced adapter. To this end, a group of RTT’s was trained to contour male
pelvic organs on planning-CTs. The objective of the study was to evaluate our
training methodology by analysing differences in contours defined by the
advanced adapter compared to the approved contours by the radiation-oncologist.
Material and Methods
In this retrospective study, planning CTs of thirty
prostate cancer patients were included. All approved contours relevant for adaptive
radiotherapy (prostate, seminal vesicles, rectum and bladder) were transferred
to Eclipse (Varian Medical Systems, Palo Alto, CA) and subsequently masked. Six
advanced adapters re-contoured these organs. Resulting contours were compared with
the approved contours. In addition, Dice similarity coefficient (DSC), volume
changes and Center of Mass (CoM) were calculated with respect to the approved
contours.
Results
The DSC was 0.96 ± 0.01 (bladder), 0.87 ± 0.06
(rectum), 0.83 ± 0.06 (prostate) and 0.73 ± 0.10 (seminal vesicles). For
rectum, the main difference was seen in the most cranial and caudal part of the
rectum. When only the part of the rectum adjacent to the PTV was measured, the
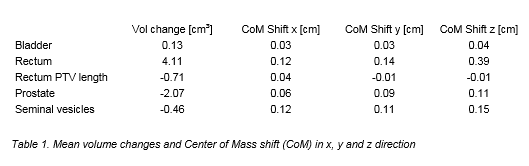
DSC improved (0.92 ±0.03) and the difference in volume diminished (Table 1).
For the seminal vesicles DSC was the lowest of all structures. Since the
seminal vesicles often had a small volume (10.07 ± 4.78 cm³), a small deviation
resulted in a lower DSC.
Conclusion
The organs
contoured by the advanced adapters and the radiation oncologists were shown to
be in excellent (bladder and rectum) or good (prostate and seminal vesicles) agreement.
This study demonstrates that transition of this work from radiation oncologist
to RTT is qualitatively feasible. Furthermore it facilitates a more efficient
distribution of the workload in the department.