The power of migration - PDF Version
“This country has benefited immensely from the fact that
we draw people from all over the world.” Alan Greenspan
I realised during a history lesson how important it could be to undertake part of my education abroad, when I learned that the so-called “Estrangeirados”, or “Europeanised” Portuguese intellectuals who had lived abroad after the late 17th century, strived to introduce the ideas of the Scientific Revolution and the Enlightenment to my home country [1]. Examples of migration benefits across history are otherwise countless. It was with that spirit in mind that, as a medical student, I took every (clinical/research) exchange opportunity that was offered during my holidays. However, the driver of my residency in Switzerland was different. It was love; this is in line with emerging literature confirming it as the main reason for mobility within Europe in recent years [2]. While working as a consultant, I decided to pursue my teenage dream, which has been fulfilled now as I am a postdoctoral research fellow in paediatric proton therapy at Massachusetts General Hospital (MGH), Harvard Medical School (HMS), in Boston, USA (Fig. 1).

Fig. 1 First visit to Massachusetts General Hospital,
January 2020 (photo credit to my very supportive husband)
Meeting the legends
“Luck is what happens when preparation meets opportunity.” Seneca
What an honour it is to learn from some of the greatest! I am blessed to hear their stories and experience history first-hand. Among others, I have learned from Norbert Liebsch, MD, PhD, a world expert in the treatment of base-of-skull sarcomas, who served at MGH from 1987, the year I was born, and who worked across the corridor until recently. The non-stop inquisitive Bernie Gottschalk, PhD, who together with Andy Koehler, BA, and colleagues, developed scattered proton beams at the Harvard Cyclotron Lab. The visionary and always charming Herman Suit, MD, DPhil, the first chief of radiation oncology at MGH, where he pioneered and fostered the use of proton therapy for cancer patients. Despite the large size of the department, which has different centres, I have always felt it was familiar. Several events would enable meetings with former and current co-workers, such as the above authorities in the field, who with more than 80-year-young experience, have more curious minds than many. The last meeting took place at the Goitein conference room (Fig. 2), named after Michael Goitein, PhD, who in collaboration with the above, developed the multifield fractionated proton therapy clinical programme and contributed extraordinarily to progress in radiation oncology [3]. Even though I never had the pleasure of meeting him personally, I feel that I know a part of him through those he worked with: from Tony Lomax, PhD, at the Paul-Scherrer Institute (PSI), who fondly remembers his personality, to Dr Herman Suit in Boston, who praises his geniality. I began working with protons while hearing about his achievements (he sadly passed away exactly when I started working at PSI), thus making me feel at home when I entered the Francis H. Burr Proton Center in January 2020 and saw the Goitein conference room, where his legacy continues.

Fig. 2 Celebration of the final patient treatment that was conducted before lockdown with double-scatter protons at the Francis H. Burr Proton Center, February 2020. On my right, Bernie Gottschalk; on my left, Dr Herman Suit; above, in the picture, Michael Goitein (photo credit to the always helpful Rachel Strauss).
The lockdown
“To achieve great things, two things are needed: a plan and not quite enough time.” Leonard Bernstein
On the evening of 11 March, the announcement that US borders had been closed caught the world by surprise. My husband now had fewer than 24 hours to join me, otherwise we would still be apart – as so many couples across the globe have unfortunately had to remain. Despite the odds, he made it happen.
When he arrived, the hospital announced the switch to remote work for thousands of employees that would begin the following day. Every employee was informed and updated through several channels (e.g., email, virtual town hall, newsletter, guidelines, video, SMS, webinar, podcasts) and section levels (i.e., departmental, clinical, research, hospital, enterprise, faculty, university), with information provided in various languages, with Q&A option in every session, all of which were recorded to make them available to the entire workforce. Soon the conferences, either clinical (e.g., tumour boards, radiological conferences, chart or proton rounds), or educational (e.g., resident morning conferences, medical rounds, career development sessions) were transitioned into virtual form – therefore they became easier to attend, especially the ones from different campuses.
You could smell the fear of the unknown when businesses started to close. It was in this environment that we moved in and furnished an apartment in record time, knowing that online shopping delivery would experience considerable delays in the coming weeks. Anxiety, together with the numbers of COVID-19 cases, was rising. We feared for our families and friends across the globe, and expected to be called at any time, as I had volunteered to help in the hospital.
Even though the Swiss Cancer Research Foundation sponsors my fellowship, uncertainty grew. There were either hiring freezes or layoffs everywhere, and the abrupt shutdown of non-COVID-related research threatened investigators with the loss of their grants. Luckily, as my main project was focused on the database from the prospective cohort of the Paediatric Proton/Photon Consortium Registry, I could continue to work around the clock, despite not knowing whether I would need to leave everything and return home earlier than expected. Close to the International Society of Paediatric Oncology abstract submission deadline, I was reassured that I was doing the right thing: my Swiss sponsor informed me that a foundation that wished to remain anonymous had decided to support my grant. This was no different from the initial plan, but was a sign of the importance of philanthropy, especially amid a pandemic when the ultimate goal is to improve the life of cancer survivors. I decided to use stress in my favour, so we submitted the project, which won the 2020 Young Investigator award. This was all thanks to the support of the MGH paediatric radiation oncology clinical research team, under the great leadership of Torunn I. Yock, MD at MGH (Fig. 3).

Fig. 3 MGH paediatric radiation oncology clinical research team in virtual mode (screenshot credit to my mentor, Dr Yock).
On 22 June, the US administration suspended the issuance of certain J-, H-, and L- visas, and banned groups of visa holders from entering the country. More than a pandemic, politics locked us down. Despite this instability, I learned many years ago with a cancer survivor (my mother) that one should not suffer in anticipation of what might be. Therefore, I will continue to do my best to not allow normal stress reactions to turn into distress, so that I can continue to focus and accomplish what I have set myself to do in the time I have left.
“Boston Strong – MGH Proud”
“We expect this to be a marathon, not a sprint.” Peter Slavin, MGH president
Boston is not new to a crisis. After 9/11, the Boston Marathon bombing, and the severe acute respiratory syndrome (SARS) epidemic, the incident command centre had helped the hospital to continue its mission. The healthcare company Mass General Brigham, together with the city of Boston and the support of the state of Massachusetts, did a tremendous job in bringing the civic, healthcare and research communities together to fight the same cause. COVID-19-specific task forces were set up throughout the system, and these with several other measures led to the creation of interdisciplinary wards practically overnight. Several employees were re-assigned (including radiation oncology colleagues); various travel nurses, together with other healthcare workers, answered the call. “Boston Hope”, a 1000-bed field medical centre, was created in six days to take pressure off the medical system in Eastern Massachusetts as COVID-19 numbers surged, as well as to give shelter and free care to the homeless. Some early achievements were celebrated, such as obtaining one million N95 masks from China with the help of the American football team, the New England Patriots, on 2 April [4], as well as a massive machine that could sterilise as many as 80000 N95 masks in a single day [5], at a time when resources were scarce.
On 24 April, we reached the (first?) peak of the surge in the number of COVID-19 inpatients, with a total of 12 floors at MGH being made COVID-floors only (Fig. 4). The hospital rearrangement took place in record time, owing to amazing leadership and extraordinary interdisciplinary cooperation at several levels. So far, we have treated four patients who were known to be COVID-19 positive in the radiation oncology department; the last of these treatments was performed on 15 May. Past the surge, we are moving towards the new normal, which I hope will improve.
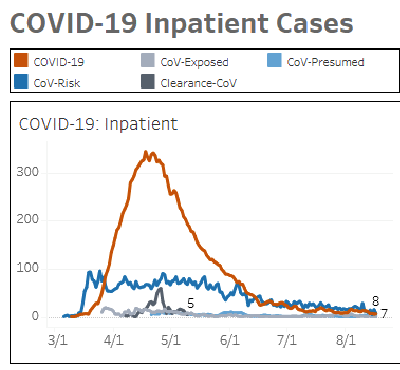
Fig. 4 Number of COVID-19 inpatients at MGH between March and June 2020. Orange line: COVID-19 confirmed across floors and intensive-care units (ICUs) (courtesy of Nancy Haff, MD, and Nino Mihatov, MD.).
At the hospital level, there is a steady decline in COVID-related activity, which enables the various recovery phases to take place slowly. It has taken a toll also on the finances of the hospital, where some contentious measures included temporary reductions in the salaries of some of its top leaders. As MGH president Peter Slavin, MD, said: “We are grateful that Massachusetts remains fairly stable, with public officials providing cautious leadership with science-based reopening plans that incorporate the opinions of experts, including many scientists from the MGH.”
Despite the adoption of remote visits, and avoidance, deferment, and the shortening of radiation therapy (RADS) frameworks [6] whenever possible, the department of radiation oncology was one of the three departments that was most clinically active at MGH throughout the crisis, which demonstrates how essential our role in clinical care is, and reminds us that cancer, just like other diseases, does not stop. I would like to highlight the rather unsung work of radiation therapists (on-site and irreplaceable, as there is no pool of hospital radiotherapists), nurses and front desk staff, among others who will continue to be on-site full time, whereas most other role groups will have a hybrid remote/on-site schedule based on department operational needs.
At a time when leadership in higher spheres is lacking, I am privileged to have witnessed it regionally firsthand. There a collective intelligence was fostered by empathetic leaders. As I learned on the Foundations of Leadership Course that I attended during last year’s European SocieTy for Radiotherapy and Oncology’s annual meeting (ESTRO38), more than a task force, a team was created among the hospital and community workers, who were linked for a common purpose, with complementary skills, hopefully to function together on a long-term basis.
«We Can Do It Together!»
Practically overnight, normal operations were disrupted, and everyone worked together to respond to this unprecedented public health crisis. Inspired by a photo of two surgical residents posing like Rosie the Riveter in a rehash of a 1940s poster, the artist Antonio Reonegro dedicated a painting called “We Can Do It Together!” to all MGH workers who had cared for patients during the COVID-19 surge (Fig. 5). The faces of these frontline workers are predominantly female, as is often the case in healthcare.

Fig. 5 Antonio Reonegro's new painting is dedicated to MGH health care workers who helped through the pandemic (courtesy of Antonio Reonegro).
Besides the gender pay gap that has widened in various sectors (in 2020!), this pandemic seems to have widened the gender gap in academic medicine as well. The proportion of first authors who were women dropped by an estimated 14% for COVID-19 papers from the number that would have been expected, based on the number of women who had written papers that were published in the same period of 2019. The main fall was observed between March and April, when the number of publications by women was 23% lower than in the same period of 2019 [7]. As Reshma Jagsi, MD, DPhil and a senior author, explained in a media release, “we suspect school closures, limited childcare and work-related service demands might have taken the greatest toll on early career women, especially during the height of the disruptions”.
As in any crisis, disparities increase. The US was no exception. The challenge is getting a splintered America to act as one. From systemic racism tangled with income inequality, this pandemic has called attention to deep-rooted inequities, and it is our moral responsibility to act to balance society.
In a see/hear/act approach, society mobilised (in the form of individuals, associations, departments, hospitals, companies, universities) to reach towards this goal. New to me was how a hospital could be such an important civic stakeholder and use good communication approaches with patients and employees to boost inclusive disability resources. Different measures were taken at each point of the chain to help reinforce health equity in every sphere, which covered:
- employees (e.g., through access to additional resources that included a range of virtual support tools, services and programmes, such as backup childcare options, wellness, work/life resources for coping with COVID-19 and recovery, storytelling, empowered bystander education and enhanced dependent-care support);
- researchers (the Mass General Brigham Center for COVID Innovation, created in record time, is a good example of successful working together with and for the healthcare community);
- patients (e.g., through enhanced interpreter services and device use, translation of COVID-19 info into several languages, post-ICU care for COVID-19 survivors’ recovery, and the empowerment of patients to register to vote while at the hospital);
- community (e.g., the transformation of hotels in hotspot communities into housing for outpatients who were unable to self-quarantine safely or effectively, management of offers and donations to red-flag communities/institutions, tablet donations, creation of a multilingual registry, supply of care kits, education campaigns, combined with identification of, mitigation of effects on, isolation of and phone communication to the vulnerable);
- society (e.g., anti-racist recovery movement, philanthropist mobilisation, advocacy in higher spheres).
I agree with Dr Slavin, who said: “I prefer the term ‘physical distancing’ [to social distancing]; it seems we need social connections now more than ever.”
Socially connected while physically distancing
“Impossible is nothing.” - Muhammad Ali
Even though I miss physical interaction with family, friends, colleagues, and my office mates, I am privileged in not having to commute and not being digitally excluded (as so many people are who do not have a proper internet connection, have one device for an entire household if at all, or are not able to connect on their own).
Until we can travel and meet with fewer risks, let’s focus on what we can control. Social events for the moment take place online. In narrow circles, we can create a sense of community with a small group of neighbours. The elimination of geographical barriers by the creation of e-meetings allows me to engage more in different associations and professional societies worldwide, and to ‘attend’ more scientific meetings. With a shift from onsite to virtual teaching/mentoring/coaching programmes, I can participate either as an attendee or as a facilitator. Through attendance at these webinars, or meet-up groups, I can network.
Life doesn’t stop. Adapt; if you cannot on your own, reach out for help. Be the agent of change and spread the love, not the virus.

Dora Correia
Radiation Oncologist, MD
Postdoctoral research fellow
Massachusetts General Hospital
Harvard Medical School
Boston, Massachusetts, USA
Twitter: @The_PT_Explorer
https://www.linkedin.com/in/doracorreia
References:
- Carneiro, A., & Simões, A. (2000). Enlightenment Science in Portugal: The Estrangeirados and their Communication Networks. Social Studies of Science, 30(4), 591–619. https://doi.org/10.1177/030631200030004004
- Gaspar, Sofia (2008), “Towards a definition of European intra-marriage as a new social phenomenon”, CIES e-Working Paper, 48, CIES-IUL, Lisbon, online at http://hdl.handle.net/10071/725 [cited 2020-08-19]
- Suit H, Chen G, Bortfeld T, et al. Michael Goitein, 1939-2016: A Giant of Modern Medical Physics. Int J Radiat Oncol Biol Phys. 2017;97(4):654-658. doi:10.1016/j.ijrobp.2016.12.032
- Shapiro M. Patriots' team plane transporting 1.2 million N95 masks from China to United States [Internet]. New York: Sports Illustrated; 2020 Apr 2 [cited 2020-08-19]. Available from: https://www.si.com/nfl/2020/04/02/patriots-team-plane-n95-masks-china-transport.
- Ostriker R. Boston hospitals getting ‘game-changer’ machine that sterilizes 80 000 protective masks a day [Internet]. Boston: Boston Globe; 2020 Apr 2 [cited 2020-08-19]. Available from: https://www.bostonglobe.com/2020/04/02/metro/boston-hospitals-getting-game-changer-machine-that-sterilizes-80000-protective-masks-day.
- Zaorsky NG, Yu JB, McBride SM, et al. Prostate Cancer Radiotherapy Recommendations in Response to COVID-19 [published online ahead of print, 2020 Apr 1]. Adv Radiat Oncol. 2020;5(4):659-665. doi:10.1016/j.adro.2020.03.010
- Andersen JP, Nielsen MW, Simone NL, Lewis RE, Jagsi R. COVID-19 medical papers have fewer women first authors than expected. eLife. 2020;9:e58807. Published 2020 Jun 15. doi:10.7554/eLife.58807